By Dr. David Edward Marcinko; MBA MEd
http://www.DavidEdwardMarcinko.com
***

***
The Impact of Medical Equipment Tariffs on Healthcare Systems
Tariffs on medical equipment have become a contentious issue in global trade and healthcare policy, particularly in the United States. These import taxes, designed to protect domestic industries and generate government revenue, can have unintended consequences when applied to essential healthcare supplies. As the U.S. healthcare system relies heavily on imported medical devices, consumables, and components, tariffs can significantly affect costs, accessibility, and innovation.
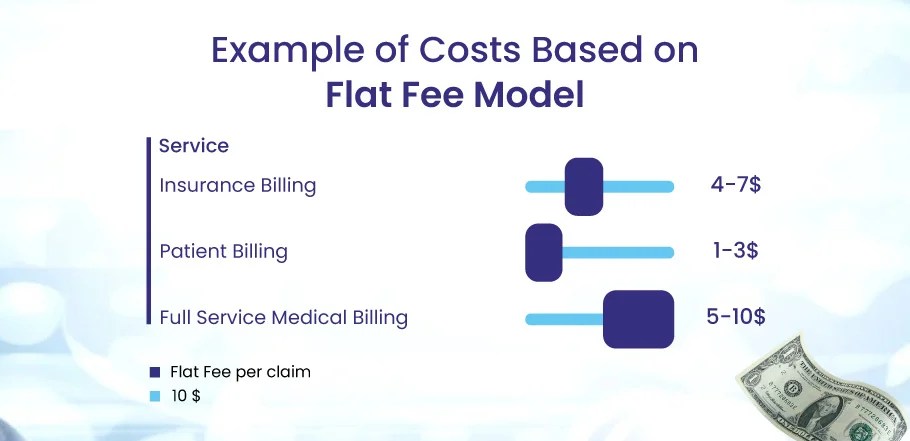
One of the most immediate impacts of medical equipment tariffs is the increase in operational costs for hospitals and healthcare providers. According to the American Hospital Association, the U.S. imported nearly $15 billion in medical equipment in 2024, much of it from countries like China. Recent tariff hikes on items such as syringes, respirators, gloves, and medical masks have raised concerns about affordability and supply chain stability. These cost increases are particularly burdensome for rural hospitals and smaller health systems, which operate on tighter budgets and have less flexibility to absorb price shocks.
Tariffs also disrupt supply chains by introducing unpredictability into procurement strategies. Unlike market-driven price changes, tariffs are policy-based and often implemented with little warning. This volatility can affect everything from disposable supplies to high-tech imaging equipment. Long-term contracts may temporarily shield hospitals from tariff impacts, but as these agreements expire, renegotiations often reflect the new cost realities. Manufacturers, in turn, may respond by relocating production, adding surcharges, or reducing product lines to manage tariff-related risks.
Beyond cost and logistics, tariffs can hinder innovation in the medical field. Many U.S.-based manufacturers rely on imported components to build advanced medical devices. When these parts become more expensive due to tariffs, companies may scale back research and development or pass costs onto consumers. This can slow the adoption of cutting-edge technologies and reduce the competitiveness of domestic firms in the global market.
***
***
From a policy perspective, the rationale for imposing tariffs on medical equipment is often rooted in national security and economic protectionism. However, critics argue that such measures may weaken health security by limiting access to critical supplies during emergencies, such as pandemics or natural disasters. The National Taxpayers Union has emphasized that tariffs on personal protective equipment and other medical goods can undermine preparedness and increase vulnerability.
To mitigate these challenges, healthcare systems and policymakers must explore strategic solutions. These include advocating for tariff exemptions on essential medical supplies, diversifying sourcing strategies, and investing in domestic manufacturing capabilities. Additionally, standardizing procurement practices and implementing cost-saving measures can help health systems navigate tariff-related pressures more effectively.
In conclusion, while tariffs may serve broader economic goals, their application to medical equipment demands careful consideration. The stakes are high—not just in terms of dollars, but in the quality and accessibility of patient care. A balanced approach that protects domestic interests without compromising health outcomes is essential for a resilient and equitable healthcare system.
COMMENTS APPRECIATED
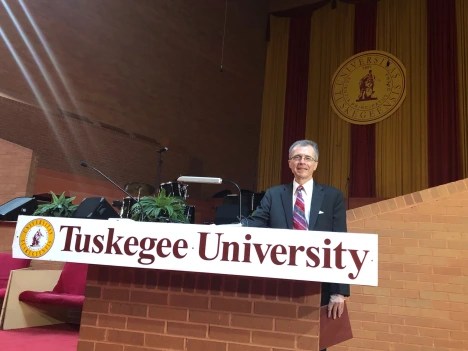
SPEAKING: ME-P Editor Dr. David Edward Marcinko MBA MEd will be speaking and lecturing, signing and opining, teaching and preaching, storming and performing at many locations throughout the USA this year! His tour of witty and serious pontifications may be scheduled on a planned or ad-hoc basis; for public or private meetings and gatherings; formally, informally, or over lunch or dinner. All medical societies, financial advisory firms or Broker-Dealers are encouraged to submit an RFP for speaking engagements: CONTACT: Ann Miller RN MHA at MarcinkoAdvisors@outlook.com -OR- http://www.MarcinkoAssociates.com
Like, Refer and Subscribe
***
***
Filed under: "Ask-an-Advisor", Ask a Doctor, Drugs and Pharma, Glossary Terms, Health Economics, Health Insurance, Health Law & Policy, Healthcare Finance, Managed Care, Management, Marcinko Associates | Tagged: AHA, American Hospital Association, chemistry-lab-equipment, david marcinko, healthcare tariffs, lab-equipment, laboratory-equipment, medical, medical equipment, medical tariffs, Science, supply chain | Leave a comment »