Tools for Transforming Our Healthcare
By Matias A. Klein
[VP, General Manager, Clinical Quality and Collaboration, Portico Systems]
 The patient-centered medical home (PCMH) continues to attract increasing attention from many industry stakeholders. The PCMH model has the potential to enhance the US healthcare system by rejuvenating primary care in a way that improves clinical outcomes, lowers costs, promotes wellness, and increases patient and physician satisfaction.
The patient-centered medical home (PCMH) continues to attract increasing attention from many industry stakeholders. The PCMH model has the potential to enhance the US healthcare system by rejuvenating primary care in a way that improves clinical outcomes, lowers costs, promotes wellness, and increases patient and physician satisfaction.
PCMH Pilot Programs
PCMH pilots are currently being tested in almost all states, including a 3-year Medicare medical home demonstration project overseen by the Centers for Medicare & Medicaid Services. However, few organizations have scaled the PCMH across their entire healthcare network, and the existing implementations appear to remain focused on care management at the expense of patient wellness. The value of focusing equally on promoting wellness (although an underappreciated nuance in the implementation of a PCMH) is a critical factor in effectively leveraging the PCMH model to improve clinical outcomes and the US healthcare system.
Centered on the Patient
The PCMH model, as its name suggests, is centered on the patient. The underlying thought is that if a comprehensive, longitudinal view of a patient is taken throughout a patient’s lifespan, the patient’s health could be better “managed” and better aligned with best medical practices. It is well documented that physicians do not consistently or frequently apply evidence based, recommended care to patients. Therefore, a major goal of the PCMH model is to improve the consistent application of evidence-based guidelines and best practices, by making longitudinal information about the patient available to providers and to patients – including any risks and recommended “intervention opportunities.” And although adherence to best practices in disease management is crucial, the PCMH model also focuses on preventing costly episodes by promoting and incentivizing wellness.
PCPs = Medical Homes
To effectively manage a patient’s health and promote wellness, primary care physicians – designated as medical homes – need to act as health “quarterbacks” or “coaches.” In such a role, these physicians will assist in aggregating a patient’s health information, making best practices transparent, offering health education and counseling, as well as coordinating the provisioning of any healthcare services the patient may need. With physicians spending significant time coaching and making critical clinical decisions, these services will be delivered with the support of care management nurses, who will handle the majority of the information processing and operational activity.
An Innovation in Care
The PCMH model is an important innovation in care delivery and has the potential to reduce medical and administrative costs, while improving the quality of care. However, how to implement the PCMH model within a care-delivery system remains unclear. Providers need the requisite infrastructure and capabilities at their locations to meaningfully participate in a PCMH. Patients must be engaged over long periods of time in proactively managing and improving their health. Outcomes and quality must be objectively measured to optimize the delivery of best possible patient care.
Potential Value
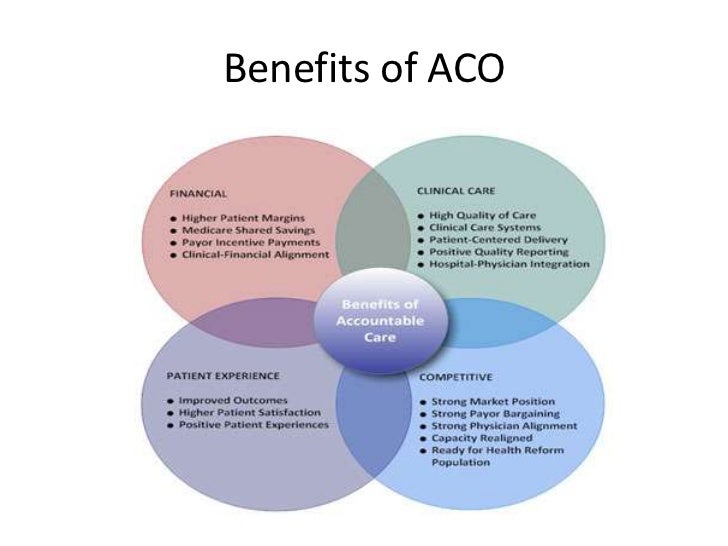
To realize the potential value of the PCMH, three distinct stakeholders – patients, providers, and health plans – must work in a collaborative way. Getting these stakeholders synchronized (i.e., aligned in their goals, using interoperable tools, and collaborating on an operational level) is no small feat but can be accomplished with the smart application of technology. Bringing these three stakeholder groups together on a common, collaborative technology platform results in what some are beginning to call the integrated PCMH. The integrated approach to the PCMH can best ensure that implementing a PCMH model does not create additional administrative burdens to health plans or provider organizations.
An integrated PCMH provides a framework for stakeholders to collaborate in a transparent fashion, and where quality, best practices, and outcomes are incentivized. The integrated PCMH also provides a pathway being awarded a medical home designation.

Vertical Integration Deployment
The key to deploying an integrated PCMH is an end-to-end vertical integration of the care-delivery process – that is, a process in which the provider network management, automation, information exchange, and analytics solutions are tightly integrated with patient and provider information. With so much complexity and so many “moving parts” in the delivery of the PCMH model, this end-to-end vertical integration is a practical solution that enables effective coordination of care and accurate measurement of quality: with such system integration, the provider network (e.g., the health plan) can bring economies of scale to even the smallest provider offices to optimize the quality of care delivery.
The 5 Keys
The five key components for such an integrated PCMH are:
- A source-of-truth for mapping medical home – designated providers, patients, as well as the associated relationships with health plans and other medical professionals; a central medical home fact checking is critical for effectively identifying, managing, and communicating with medical home and their networks.
- A set of collaborative workflows that align stakeholders with best practices, incentives, and quality measures reporting; these collaborative workflows help each stakeholder understand where a given patient is in the care-delivery process, potential intervention opportunities, why certain interventions are being emphasized, and what incentives are available for executing specific interventions.
- An infrastructure for clinical integration and distribution of intervention opportunities, clinical reference content, education, alerts, and reminders. This infrastructure allows all stakeholders to have access to up-to-date, accurate patient information; it aligns stakeholders and helps reduce or eliminate duplication of procedures and tests.
- Interoperable clinical applications and collaboration tools to enable patients and physicians to engage in medical home processes; these tools – which include electronic medical records, e-prescribing, e-labs, secure e-mail, personal health records, and document management and exchange technology – can help manage health information, assist with decision-making, and improve communication between patients, providers, and health plans.
- Incentive management and analytics tools for modeling, setting, measuring, and rewarding incentives based on quality measures and outcomes; these tools must span the entire PCMH delivery process and are required for objectively evaluating and optimizing the performance of a medical home.
When considering the multiplicity of stakeholders, information, software systems, and knowledge that has to be coordinated in the context of a PCMH model, implementing a medical home pilot and scaling it to a full-blown network may seem a daunting task. The integrated PCMH offers a real-world solution for deploying a scalable and flexible infrastructure for the management of this emerging care-delivery model.
Assessment
Early evaluations of the PCMH model show promising, albeit inconclusive, outcomes. The integrated PCMH model offers a practical road map for deploying a management system that will enable objective measurement of PCMH performance and outcomes.
Conclusion
Although the jury is still out on the ultimate value of the PCMH, deploying an integrated PCMH system can help position PCMH pilots in a way that enhances their flexibility and scalability to support full-scale network transformation.
Your thoughts and comments on this ME-P are appreciated. Feel free to review our top-left column, and top-right sidebar materials, links, URLs and related websites, too. Then, subscribe to the ME-P. It is fast, free and secure.
Speaker: If you need a moderator or speaker for an upcoming event, Dr. David E. Marcinko; MBA – Publisher-in-Chief of the Medical Executive-Post – is available for seminar or speaking engagements. Contact: MarcinkoAdvisors@msn.com
OUR OTHER PRINT BOOKS AND RELATED INFORMATION SOURCES:


Filed under: "Doctors Only", Book Reviews, Career Development, Managed Care, Practice Management, Quality Initiatives, Research & Development | Tagged: CMS, Matias A. Klein, Patient Centered Medical Home, Portico Systems, The Integrated Patient-Centered Medical Home Model | 6 Comments »