My Search for Truth – 2009
[By Darrell Kellus Pruitt; DDS]
Do the leaders of the American Dental Association [ADA] encourage critical thinking by membership? Or; do they fear my opinion of what appears to be destructive and self-serving institutional bias in my ADA that favors businesses peripheral to the care of dental patients, and at patients’ expense? I think it is clear that there are a few good ol’ boys imbedded in the fat ADA who prefer to hide behind a comfortable, but obsolete command-and-control ADA business model. The mighty ostrich stuck its head in the sand. Then along came a noisy, gasoline-powered weed-whacker. Never saw it coming.
Evidence-Based Dentistry Champion Conference
On May 29-30, the First Annual “Evidence-Based Dentistry (EBD) Champion Conference” will be convened in ADA Headquarters in Chicago. Just like last year, the meeting with a brand-new name is sponsored by Procter & Gamble and The Journal of Evidence-Based Dental Practice with Dr. Michael G. Newman as its Editor and Chief. Even though this effort is enthusiastically supported by large corporations with products to sell, like P&G, managed care insurance companies such as Delta Dental, and electronic health records vendors such as Allscripts, the power of the reclusive stakeholders is further amplified by bureaucrats inside and outside the ADA – siphoning off my professional organization’s credibility. That is my opinion based on actual contact with a few characters in this group.
Evidence-Based Dentistry: 3rd International Conference
I attended the meeting last year when it was called “Evidence-Based Dentistry: 3rd International Conference” – I assume that in the last year, it lost its “international” status, and now caters only to “EBD Champions” (cheerleaders). Last year, they were also looking for Champions for their EBD ideas, but the bias was better concealed. I reported on the meeting in an article called “Evidence-Based Dentistry – My search for truth.”
http://community.pennwelldentalgroup.com/forum/topics/evidencebased-dentistry-my
Shortly into the meeting on May 4, 2008, I could tell by a show of hands from attendees that as a dentist who actually puts his hands in patients’ mouths as a regular part of his job; I was virtually alone in the auditorium. This was confirmed by the volume of “Boo” directed at me later that day. The Champions who had been selected months before the conference had already met that week and they were pumped. One could smell the zeal for EBD – whatever it means.
Journal of Evidence-Based Dental Practice
In his introduction to last year’s conference, Dr. Michael G. Newman, Editor in Chief of the Journal of Evidence-Based Dental Practice, told attendees that P&G is providing all the information about EBD to all the dental schools in the nation. I will be honest with you. Being booed last year for addressing what I think is the inferior quality of managed care dentistry during the final discussion period may have affected my attitude about EBD. In addition, being subsequently blocked from responding to a hurt and angry managed care discount dentistry broker by an ADA employee named Dr. Ron Zentz also disappointed me in my ADA. Dr. Zentz told me “This is not the place for this” as he stood between me and the microphone. Later I could not get Zentz to concede the indisputable fact that quality is proportional to reward. When I pressed him for an answer to the managed care question, he stoically repeated exactly what the insurance representative said: “Whether the dentistry is managed care or not, it makes no difference in the quality of care.” Here is something cute: The event was an “Evidence-Based” conference on the second floor of the Headquarters of the ADA, and Dr. Zentz is employed in the ADA’s “unbiased” science department. Get it? Now that’s funny!
Trouble-Makers Don’t Get Invited Back
My bad behavior last year may have something to do with why I was not invited to attend this year, even though I worked hard on the prerequisite essays which I will share with you later. Nevertheless, I have to warn that ADA-approved propaganda from P&G doesn’t strengthen this dentist’s confidence that our leaders are protecting the future of dentistry, friends. Take a look at what healthcare parasites have quietly done over the last decade or so to physicians’ practices with the blessing of the AMA, and counter to the interests of patients. Those same parasites were in ADA Headquarters on May 4, 2008. Our house at 211 East Chicago Avenue reeked.
EDB Vagueness
Like the HIPAA Rule on which Newman’s favorite interpretation of EBD leans hard, the beauty of EBD is in its vagueness. Both HIPAA and EBD can mean damn well anything one needs them to mean, and stakeholders with lots of influence have their fingerprints and drool all over the plans. For example, Dr. Robert Ahlstrom, a stakeholder and one of the speakers at last year’s conference uses HIPAA to support EBD and vice-versa according to closed-circuit, cause-I-said-so science that he evidently makes up as he goes. It is difficult for me to imagine that Ahlstrom’s eleven reasons that HIPAA benefit dentistry – which he presented as testimony for HHS Secretary Michael Leavitt over a year ago – were approved by a committee. I think Ahlstrom made up his reasons while waiting in the hall for the NCVHS meeting to begin. If the reasons were indeed approved by an ADA committee, I extend my sympathy. It must be difficult for challenged people like that to safely find their way home from work every day.
(See “HIPAA and Dentistry – About Ahlstrom’s Controversial HIPAA Testimony”)
https://healthcarefinancials.wordpress.com/2009/01/08/hipaa-and-dentistry/
Where is the Evidence?
A few hours before Dr. Ahlstrom, an ADA NHII (National Health Information Infrastructure) Task Force member, took the podium, Dr. Newman pleaded with dentists to always ask, “Where is the evidence?” I know Dr. Ahlstrom heard Dr. Newman’s words because Ahlstrom was sitting on the first row, next to ADA Senior VP Dr. John Luther, who is in charge of the ADA Department of Dental Informatics – a major beneficiary of EBD and HIPAA.
***

***
Buzzwords
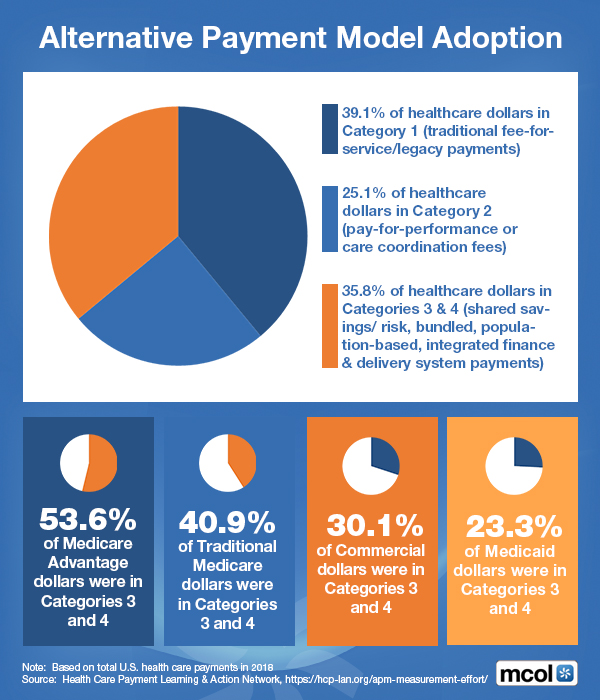
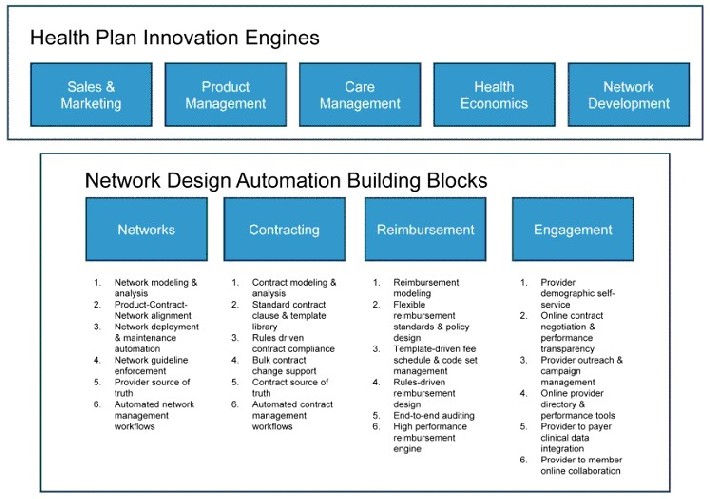
I have come to the conclusion that EBD is a buzzword for a scheme supported by avaricious stakeholders who seek to regulate dentistry using healthcare IT. I assume it will be left to Dr. Robert Ahlstrom to present the plan to the next administration in his special, fanciful way. It is clear to me that the ADA is using Ahlstrom to lead American dentists down a computerized, cook-book path initially promoted several years ago at ADA Headquarters by none other than Newt Gingrich. The path ends with the NPI, NPPES and Ingenix-style Pay-for-Performance instead of free-market competition and consumers’ desires. Like Ahlstrom, EBD is little more than a tool.
Living with Rejection
I learned a couple of days ago that my application for this year’s conference was rejected. A PDF letter signed by Dr. Michael Newman, Editor and Chief of the Journal of Evidence-Based Dental Practice stated that the competition for seats was intense this year, and that I just didn’t have what the selection committee was looking for in a “champion” – even though one can see by their essay questions that the EBD stakeholders desire dentists who can draw audiences.
My Responses
Below are my responses to this year’s questions that I posted on September 23, even before I hooked up with PennWell, and the ME-P. I’m even more widely read now.
Q: Are you involved in the treatment of populations with limited access to care?
Counseling people who have big problems and little money is part of the job. Almost every day I help patients make hard decisions that affect their appearance as well as health. Compromises are always difficult, especially when it involves children. I do my best to provide my patients with the information they need concerning their specific problems in a personal manner. In that respect, I am no different than almost all other dentists I know.
Q: Given the opportunity, how do you plan to disseminate the information and knowledge of EBD?
For dentistry-related news, I am arguably the most popular commentator on the Internet. If I am convinced that EBD is in patients’ best interest, I can promote the concept to a wider audience than anyone else in dentistry and it will not cost a thing. I can use any number of websites in addition to a private network of colleagues that has been in place for almost three years.
If I leave the conference suspecting that stakeholders ambushed EBD to manipulate dentist-patient relationships for selfish reasons, I will work even more effectively to undermine it. Fair is fair.
Q: Are there any specific examples that demonstrate your ability to be a good disseminator?
Apart from having an increasingly popular column about healthcare matters on this ME-P https://healthcarefinancials.wordpress.com/?s=darrell+pruitt+dds ), I am always seeking new and innovative ways to attract attention to dentistry. I am very good at what I do.
Here is a simple demonstration of my talent: Googlesearch “Darrell Pruitt DDS.” You will discover that I’ve got what they call “googlejuice.” I create interesting content. People you need to reach read me.
The question is; does the ADA have the confidence to subject EBD to my critique? On the other hand, does the ADA have the courage not to?
Since I will not be allowed to keep colleagues in my neighborhood as informed in real-time and in detail as they should be, I invite one or more “EBD Champions” to describe what they learned following the Conference in May right here on this ME-P and PennWell forums. And as always, I invite Dr. Robert Ahlstrom to discuss what he plans to do with my dental practice.
Assessment
Tomorrow, as part of “Transparency and the ADA – a dissecting experiment,” I intend to post another question on the EBD link following my weekly report. I will ask if Dr. Robert H. Ahlstrom will be addressing the audience before having my name put on a short-call list to replace late-cancellations. Depending on the answer, I may go camping instead.
Channel Surfing the ME-P
Have you visited our other topic channels? Established to facilitate idea exchange and link our community together, the value of these topics is dependent upon your input. Please take a minute to visit. And, to prevent that annoying spam, we ask that you register. It is fast, free and secure.
Conclusion
Your thoughts and comments on this ME-P are appreciated. Feel free to review our top-left column, and top-right sidebar materials, links, URLs and related websites, too. Then, subscribe to the ME-P. It is fast, free and secure.
Speaker: If you need a moderator or speaker for an upcoming event, Dr. David E. Marcinko; MBA – Publisher-in-Chief of the Medical Executive-Post – is available for seminar or speaking engagements. Contact: MarcinkoAdvisors@msn.com
OUR OTHER PRINT BOOKS AND RELATED INFORMATION SOURCES:



Filed under: "Doctors Only", Career Development, Ethics, Op-Editorials, Quality Initiatives, Research & Development | Tagged: ADA, Allscripts, American Dental Association, delta dental, Dr. John Luther, Dr. Michael G. Newman, Dr. Robert Ahlstrom, Dr. Ron Zentz, EBD, eDRs, evidence based dentistry, Evidence-Based Dentistry: 3rd International Conference, HIPAA, Ingenix, National Health Information Infrastructure, Newt Gingrich, NHII, NPI, NPPES, P&G, P4P, Pay-for-Performance, PennWell, Procter & Gamble, The Journal of Evidence-Based Dental Practice | 7 Comments »