Understanding the So-Called New York Protocol
By Sheri Fink
ProPublica News
With scant public input, state and federal officials are pushing ahead with plans that — during a severe flu outbreak — would deny use of scarce ventilators by some patients to assure they would be available for patients judged to benefit the most from them.
The plans have been drawn up to give doctors specific guidelines for extreme circumstances, and they include procedures under which patients who weren’t improving would be removed from life support with or without permission of the families.
The plans are designed to go into effect if the U.S. were struck by a severe flu pandemic comparable to the 1918 outbreak that killed an estimated 50 million people worldwide. State and federal health officials have concluded that such a pandemic would sicken far more people needing ventilators than could be treated by the available supplies.
VA Guidelines
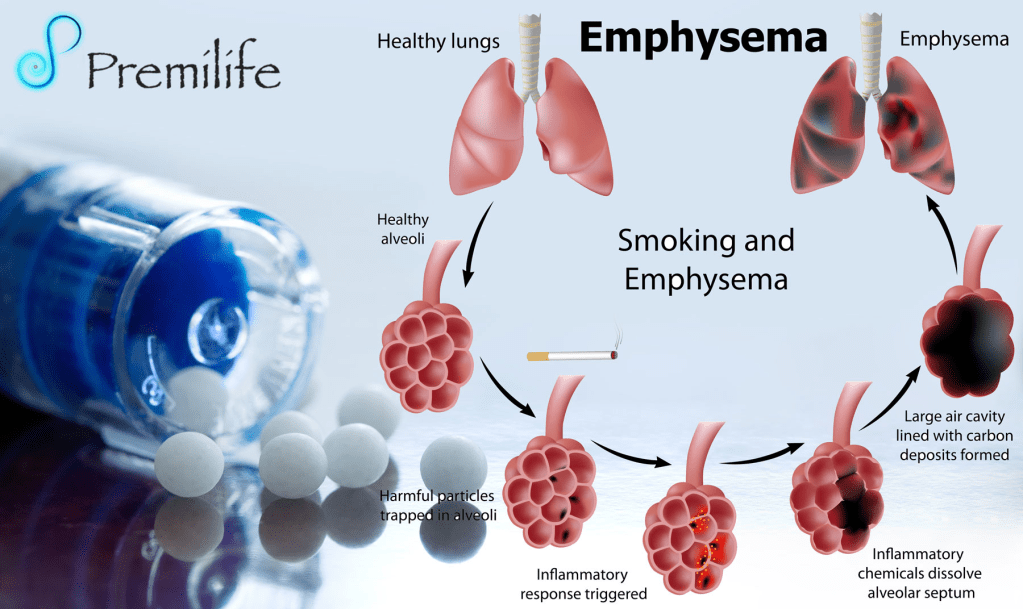
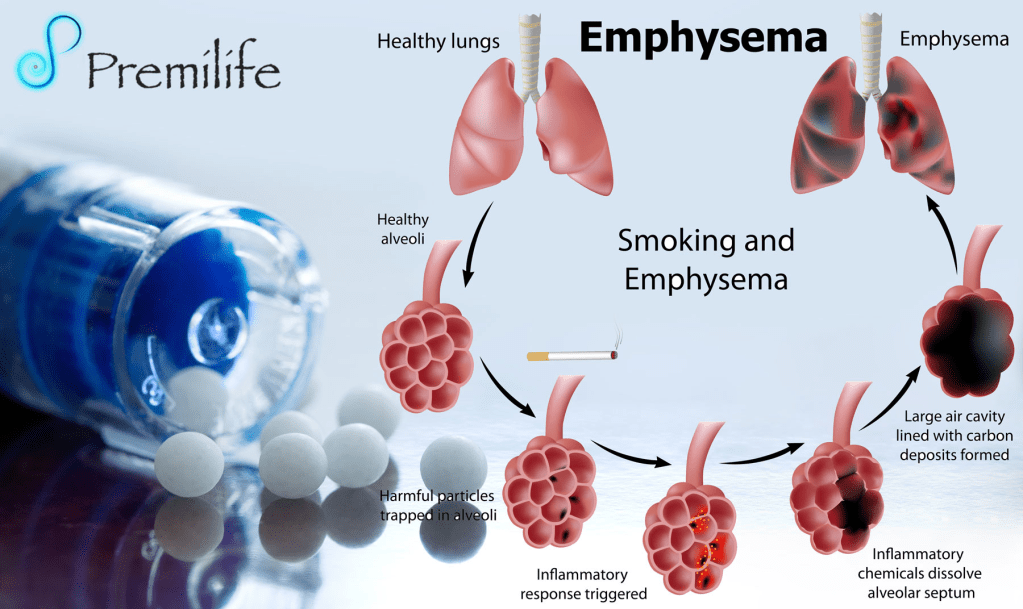
Many of the draft guidelines, including those drawn up by the Veterans Health Administration, are based in part on a draft plan New York officials posted on a state web site two years ago and subsequently published in an academic journal. The New York protocol, which is still being finalized, also calls for hospitals to withhold ventilators from patients with serious chronic conditions such as kidney failure, cancers that have spread and have a poor prognosis, or “severe, irreversible neurological” conditions that are likely to be deadly.
New York officials are studying possible legal grounds under which the governor could suspend a state law that bars doctors from removing patients from life support without the express consent of the patient or his or her authorized health agent.
Medicare Payment
State and federal officials involved with drafting the plans say they have been disquieted by this summer’s uproar over whether Medicare should pay for end-of-life consultations with families. They acknowledged that the measures under discussion go far beyond anything the public understands about how hospitals might handle a severe pandemic.
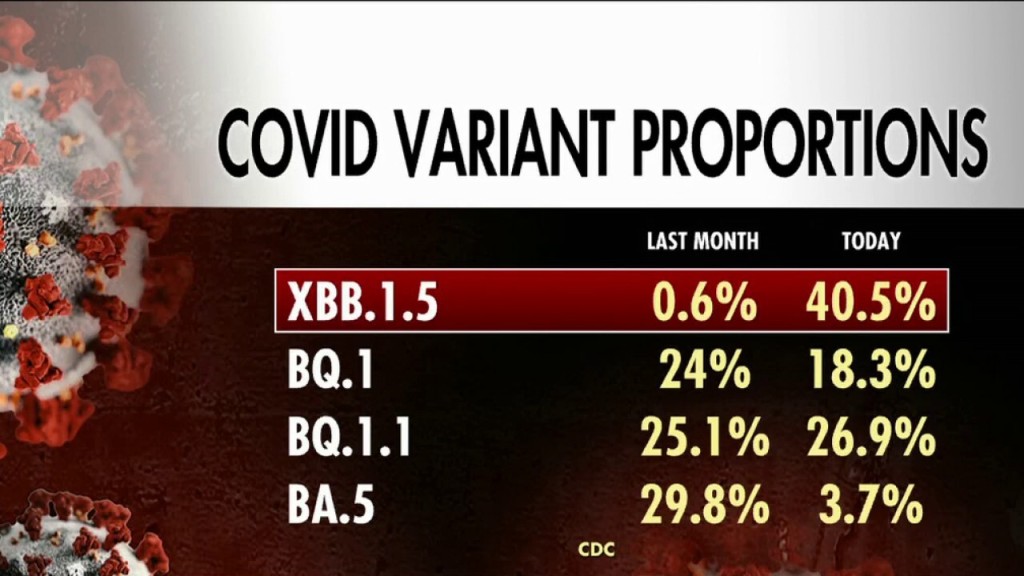
By every indication, state and federal officials expect to weather this year’s flu season without having to ration ventilators. That assumes that the H1N1 virus will not mutate into a more serious killer, the vaccines against it and the other seasonal flus will continue to prove effective, and any dramatic surges in the number of patients in need of ventilators will occur in different parts of the U.S. at different times.
In recent months, New York officials have met three times with physicians, respiratory therapists and administrators to rehearse how their plan might play out in hospitals in a severe epidemic. In one of those “tabletop exercises,” participants suggested that the names of triage officers charged with making life and death choices among patients at each hospital should be kept secret. The secrecy would be needed, participants said in interviews, to avoid pressure and blame from colleagues caring for patients who were selected to be taken off life support.
When they posted their plan on the web in coordination with a video conference in 2007, New York officials promised to solicit public input. Since then, they have consulted with medical and legal professionals and other experts, but few members of the general public, and the plan has remained unchanged. They declined to make the comments they have gathered immediately available for review, and those comments are not published on the Health Department’s Web site.
In the initial proposal, officials called public review “an important component in fulfilling the ethical obligation to promote transparency and just guidelines.”
The academic publication of the plan envisaged the use of focus groups to solicit comment from “a range of community members, including parents, older adults, people with disabilities, and communities of color.” Those have not been held.
Beth Roxland, the current executive director of the New York State Task Force on Life and the Law, said the ethicists included in the state’s planning process focused largely on vulnerable populations. “Even if we didn’t have direct input from vulnerable populations,” she said, “their interests have been well accounted for.” Roxland said that public comment solicited when the ventilator plan was posted on the Health Department Web site was “sparse.”
Dr. Guthrie Birkhead, Deputy Commissioner of the Office of Public Health for New York State said he wondered whether it was possible to get the public to accept the plans. “In the absence of an extreme emergency, I don’t know. How do you even engage them to explain it to them?”
Even so, other states, hospital systems and the Veterans Health Administration—which has 153 medical centers across all states — have drafted protocols that are based in part on New York’s plan. The inclusion and exclusion criteria for access to ventilators, however, are different. For example, under the current drafts, a patient on dialysis would be considered for a ventilator in a VA hospital in New York during a severe pandemic, but not in another New York hospital that followed the State’s plan, which excludes dialysis patients. The VA’s exclusion criteria are looser because the patient population it is charged with serving is typically older and sicker than in other acute care hospitals. Different states, reflecting different values, have also established different criteria for who gets access to lifesaving resources.
IOM Input
The Institute of Medicine, an independent national advisory body, is expected to release a report on Thursday morning, at the request of the U.S. Department of Health and Human Services, that will recommend broad guidelines to help guide planners crafting altered standards of care in emergencies. At an open meeting held to inform the report on Sept. 1, participants described successful public exercises related to allocating scarce resources in Utah and in a Centers for Disease Control and Prevention study conducted in Seattle.
Questions about how hospitals would handle massive demand for life support equipment arose when New York state health department officials ran exercises based on a scenarios involving H5N1 avian influenza.
“They kept running out of ventilators,” said Dr. Tia Powell, director of the Montefiore-Einstein Center for Bioethics and former executive director of the New York State Task Force on Life and the Law, which was asked to address the problem. “They immediately recognized this is the worst thing we’ve ever imagined. What on earth are we going to do?”
Officials calculated that 18,000 additional New Yorkers would require ventilators in the peak week of a flu outbreak as deadly as the 1918 pandemic. Only a thousand machines would be available, the officials estimated. The state’s acute care hospitals in 2005 had about 6000 ventilators, 85% of which were normally in use. A moderately severe pandemic would have resulted in a shortfall of 1256 ventilators, health officials found.
In 2006, New York planners convened a group of experts in disaster medicine, bioethics and public policy to come up with a response. After months of discussion, the group produced the system for allocating ventilators. They first recommended a number of ways that hospitals could stretch supply, for example by canceling all elective surgeries during a severe pandemic. The state has also since purchased and stockpiled 1700 Pulmonetic Systems LTV 1200 ventilators (Cardinal Health Inc., NYSE) — enough to deal with a moderate pandemic but not one of 1918 scale.
Officials realized those two measures alone would not be enough to meet demand in a worst-case scenario. Ventilators were costly, required highly trained operators, and used oxygen, which could be limited in a disaster.
Ventilator Rationing
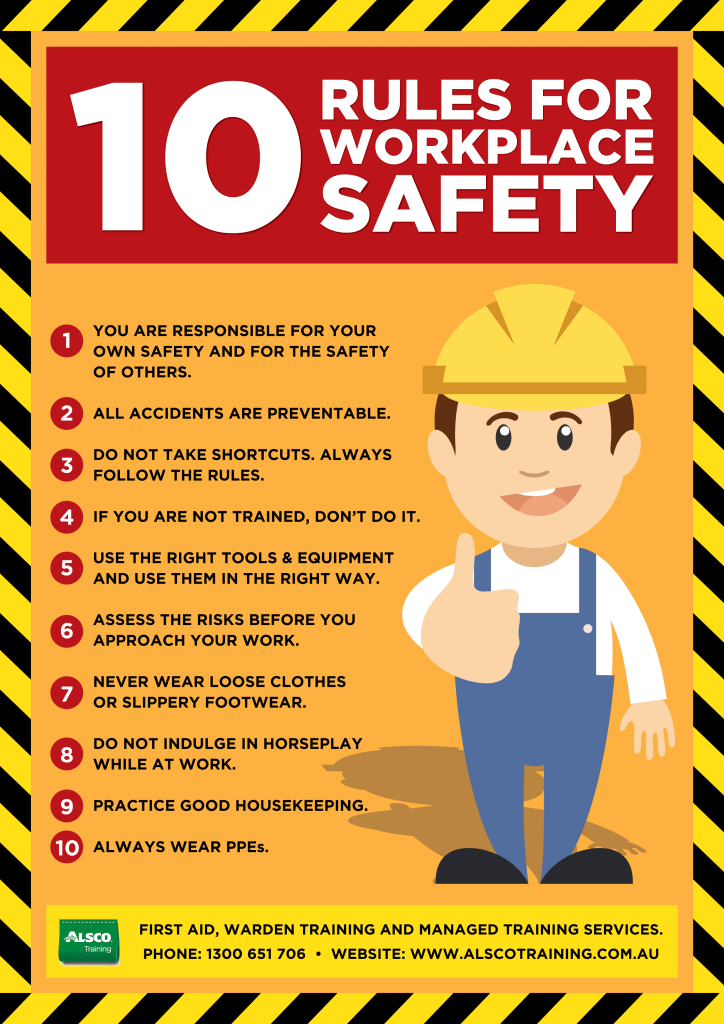
The group then drew up plans for rationing of ventilators. The goal, participants said, was to save as many lives as possible while adhering to an ethical framework. This represented a departure from the usual medical standard of care, which focuses on doing everything possible to save each individual life. Setting out guidelines in advance of a crisis was a way to avoid putting exhausted, stressed front line health professionals in the position of having to come up with criteria for making excruciating life and death decisions in the midst of a crisis, as many New Orleans health professionals had to do after Hurricane Katrina.
The group based its plans, in part, on a 2006 protocol developed by health officials in Ontario, Canada which relied on quantitative assessments of organ function to decide which patients would have preference for an intensive care unit bed. The tool, known as the Sequential Organ Failure Assessment (SOFA) score, is not designed to predict survival, and not validated for use in children, but the experts adopted it in light of the lack of an appropriate alternative triage system.
This summer, New York officials brought the state’s plan to groups from several New York hospitals for the tabletop exercises. They met behind closed doors to assess how hospitals might implement the proposed measures if the H1N1 pandemic turned unexpectedly severe this fall. In the fictional scenario, paramedics were ordered not to place breathing tubes into patients until physicians “can assess whether they meet the criteria to be placed on a ventilator.’’
Problems were immediately apparent. Dr. Kenneth Prager, a professor of medicine and director of clinical ethics at Columbia University Medical Center, was concerned about the lack of awareness of the plan among the larger public and the majority of the medical community. Societal input “is totally absent,” he said and called for more outreach to the public. “Maybe society will say, ‘We don’t agree with your plan. You may think it’s ethically OK; we don’t.'”
The Protocol
The protocol, he said, would also place a great burden on clinicians charged with selecting which patients would be removed from life support. Physicians were concerned doctors involved in the legitimate and painful selection processes might be inappropriately construed as “death squads.” “We facetiously dubbed them the ‘death squad’ or the ‘guys in the back room’,” Prager said. He envisioned family members breaking down and screaming when they found out their loved ones would be disconnected from ventilators. “It really is a nightmare.”
Even so, he felt that the plan – and its effort to save the greatest number of patients – was ethically appropriate. “If we don’t use triage, people will die who would have otherwise been saved,” he said, because a number of ventilators are “being used to prolong the dying process of patients with virtually no chance of surviving.”
Doctors at the exercises feared that they would be sued by angry patients if they followed the draft guidelines. “There’s absolutely no legal backing for physicians,” said Lauren Ferrante, a medical resident at Columbia University Medical Center. “Who’s to say we’re not going to get sued for malpractice?”
New York State law forbids doctors from removing living patients from ventilators or other life support except in cases where the patient has clearly stated such wishes, for example in a living will, or through his or her legal health care agent. Other sources of liability could come from federal and state anti-discrimination laws or claims of denial of due process.
New York officials said they were currently working out legal options for implementing the plans, such as gubernatorial emergency declarations or emergency legislation.
“You can take something today that’s not necessarily active and overnight flip the switch and make it into something that has those teeth in it,” said Dr. Powell, who served on the committee that drafted the plan.
Dr. Powell cautioned that it is critically important to maintain flexibility in the guidelines. Any rationing measures taken in a disaster must be calibrated to need and severity.
Guidelines can also promote investment in new technology, such as cheaper, easier to use ventilators that would make rationing less likely. Already at least one company, St. Louis-based Allied Healthcare Products, is marketing a line of ventilators specifically for use in disasters.
Some states, including Louisiana and Indiana, have adopted laws that immunize health professionals against civil lawsuits for their work in disasters. Other states, including Colorado, have drawn up a series of relevant executive orders that could be applied to address these issues.
Assessment
Dr. Carl Schultz, a professor of emergency medicine at the University of California at Irvine and co-editor of the forthcoming textbook, Koenig and Schultz’s Disaster Medicine (Cambridge University Press), is one of the few open critics of the establishment of altered standards of care for disasters. He says the idea “has both monetary and regulatory attractiveness” to governments and companies because it relieves them of having to strive to provide better care. “The problem with lowering the standard of care is where do you stop? How low do you go? If you don’t want to put any more resources in disaster response, you keep lowering the standard.”
Federal officials disagree. “Our goal is always to provide the highest standard of care under the circumstances,” said RADM Ann Knebel, deputy director of preparedness and planning at the Office of the Assistant Secretary for Preparedness and Response, Department of Health and Human Services. “If you don’t plan, then you are less likely to be able to reuse, reallocate and maximize the resources at your disposal, because you have people who’ve never thought about how they’d respond to those circumstances.”
Note: Sheri Fink is a reporter for the ProPublica news service, which first published this article.

Conclusion
And so, your thoughts and comments on this Medical Executive-Post are appreciated. Feel free to review our top-left column, and top-right sidebar materials, links, URLs and related websites, too. Then, be sure to subscribe to the ME-P. It is fast, free and secure.
Link: http://feeds.feedburner.com/HealthcareFinancialsthePostForcxos
Get our Widget: Get this widget!
Our Other Print Books and Related Information Sources:
Practice Management: http://www.springerpub.com/prod.aspx?prod_id=23759
Physician Financial Planning: http://www.jbpub.com/catalog/0763745790
Medical Risk Management: http://www.jbpub.com/catalog/9780763733421
Healthcare Organizations: www.HealthcareFinancials.com
Health Administration Terms: www.HealthDictionarySeries.com
Physician Advisors: www.CertifiedMedicalPlanner.com
Filed under: Breaking News, Ethics, Health Law & Policy, Quality Initiatives | Tagged: Allied Healthcare Products, Ann Knebel, bio-ethics, CDC, death squads, Disconnecting Ventilators, Dr. Carl Schultz, Dr. Guthrie Birkhead, Dr. Kenneth Prager, Dr. Powell, Dr. Tia Powell, H1N1 virus, IOM, Koenig and Schultz’s Disaster Medicine, Lauren Ferrante, medical ethics, Montefiore-Einstein Center for Bioethics, ProPublica News, Pulmonetic Systems LTV 1200 ventilators, Sequential Organ Failure Assessment score, Sheri Fink, SOFA, USDHHS, VA, Ventilator Rationing | Leave a comment »