By Dr. David Edward Marcinko; MBA MEd
SPONSOR: http://www.MarcinkoAssociates.com
***
***
A medical economic white elephant is a healthcare-related investment—such as a hospital, device, or system—that consumes vast resources but fails to deliver proportional value, often becoming a financial burden rather than a benefit to public health.
In economic terms, a white elephant refers to an asset whose cost of upkeep far exceeds its utility. In the medical field, this concept manifests in projects or technologies that are expensive to build, maintain, or operate, yet offer limited practical use, accessibility, or return on investment. These ventures often begin with noble intentions—improving care, advancing technology, or expanding access—but end up draining resources due to poor planning, misaligned incentives, or lack of demand.
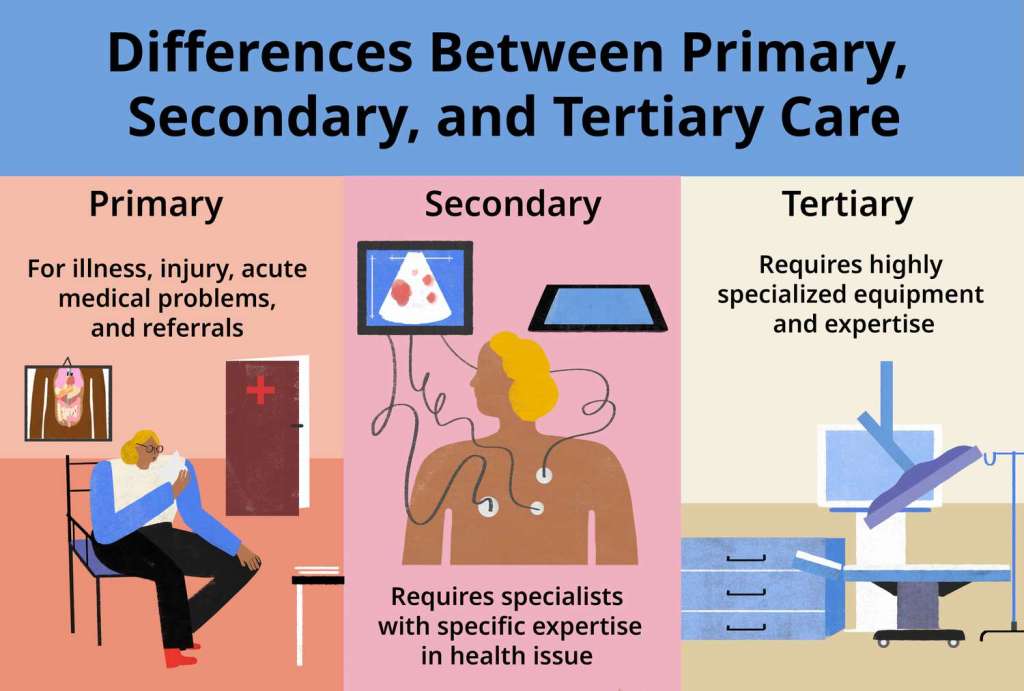
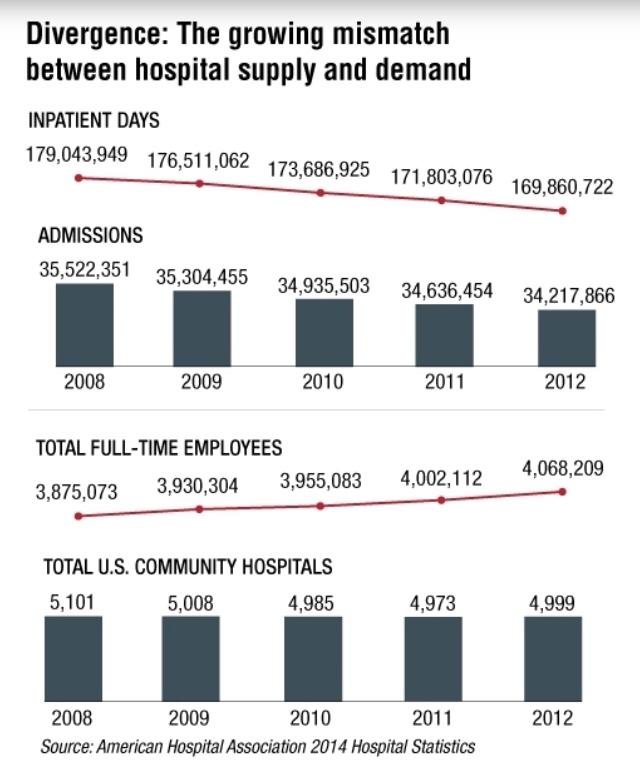
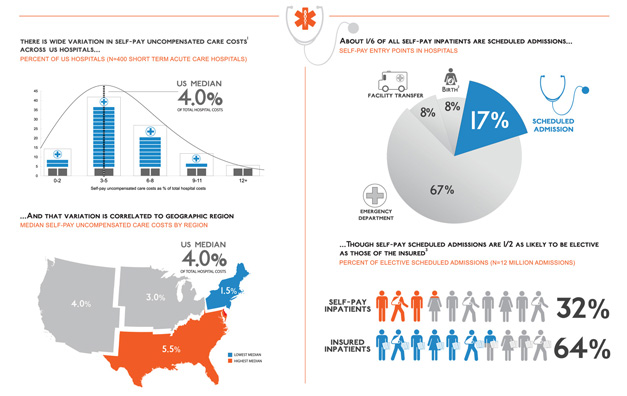
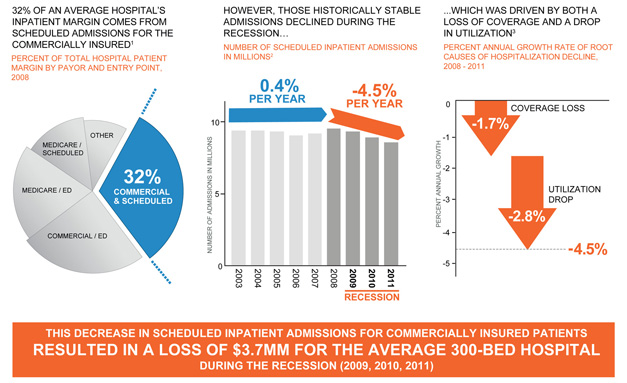
One prominent example is the construction of underutilized hospitals or specialty centers in regions with low patient volume. Governments or private entities may invest heavily in state-of-the-art facilities without conducting thorough needs assessments. The result: gleaming buildings with advanced equipment but few patients, high operating costs, and staff shortages. These facilities often struggle to stay open, becoming financial sinkholes that divert funds from more pressing healthcare needs.
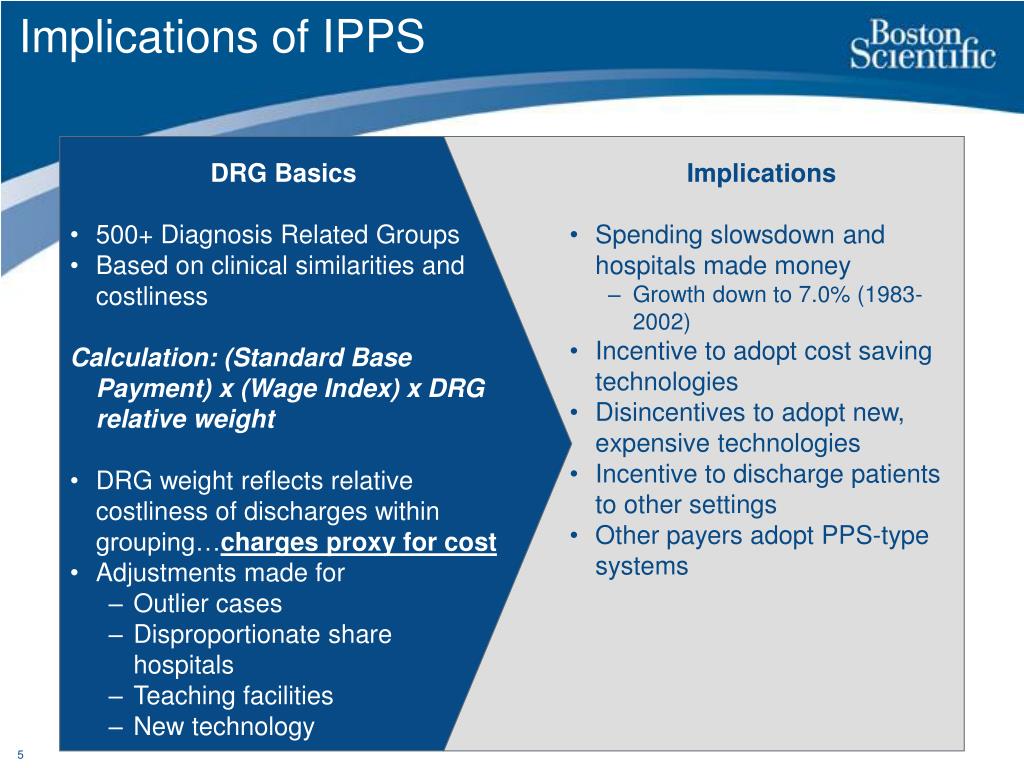
Medical devices and technologies can also become white elephants. For instance, robotic surgical systems or high-end imaging machines are sometimes purchased by hospitals to boost prestige or attract patients, despite limited clinical necessity or trained personnel. These devices require costly maintenance, specialized training, and may not significantly improve outcomes compared to traditional methods. When reimbursement rates don’t justify their use, they become liabilities.
***
***
Electronic health record (EHR) systems offer another cautionary tale. While digitizing patient records is essential, some EHR implementations have ballooned into multi-million-dollar projects plagued by inefficiencies, poor interoperability, and user dissatisfaction. Hospitals may invest in proprietary systems that are difficult to integrate with others, leading to fragmented care and wasted resources. In extreme cases, these systems are abandoned or replaced, compounding the financial loss.
The consequences of medical white elephants are far-reaching. They can strain public budgets, increase healthcare costs, and erode trust in institutions. In developing countries, such projects may be funded by international aid or loans, saddling governments with debt while failing to improve population health. Even in wealthier nations, misallocated resources can mean fewer funds for primary care, preventive services, or community health initiatives.
***
***
Avoiding medical white elephants requires rigorous planning, stakeholder engagement, and evidence-based decision-making. Health systems must assess actual needs, forecast demand, and consider long-term sustainability. Cost-benefit analyses should include not only financial metrics but also health outcomes, equity, and accessibility. Transparency and accountability are key to ensuring that investments serve the public good.
In conclusion, the concept of a medical economic white elephant highlights the importance of aligning healthcare investments with real-world needs and outcomes. While innovation and expansion are vital, they must be grounded in practicality and sustainability.
By learning from past missteps, health systems can prioritize value-driven care and avoid the costly pitfalls of overambitious or poorly conceived projects.
COMMENTS APPRECIATED
SPEAKING: Dr. Marcinko will be speaking and lecturing, signing and opining, teaching and preaching, storming and performing at many locations throughout the USA this year! His tour of witty and serious pontifications may be scheduled on a planned or ad-hoc basis; for public or private meetings and gatherings; formally, informally, or over lunch or dinner. All medical societies, financial advisory firms or Broker-Dealers are encouraged to submit an RFP for speaking engagements: CONTACT: Ann Miller RN MHA at MarcinkoAdvisors@outlook.com -OR- http://www.MarcinkoAssociates.com
Like, Refer and Subscribe
***
***
Filed under: "Ask-an-Advisor", Ask a Doctor, Drugs and Pharma, economics, Glossary Terms, Health Economics, Health Insurance, Healthcare Finance, Investing, Marcinko Associates, Practice Management, Practice Worth | Tagged: ASC, cost benefit analysis, CVPA, david marcinko, economic investments, education, EHRs, EMRs, finance, financial iunvestments, hospital investments, hospitals, Investing, Medical Devices, medical economic investments, travel, white elephamt, writing | Leave a comment »