Dr. David Edward Marcinko; MBA MEd
SPONSOR: http://www.HealthDictionarySeries.org
***
***
A Comprehensive Overview
Medicine is an extraordinarily diverse field, shaped by centuries of scientific discovery and the evolving needs of human health. As knowledge has expanded, so too has the need for physicians to specialize in particular systems, diseases, or patient populations. Today’s medical landscape includes a wide range of specialties, each with its own philosophy, diagnostic approach, and therapeutic focus. Understanding these specialties not only clarifies how modern healthcare functions but also highlights the complexity of caring for the human body. The following essay explores twenty major medical specialties, defining their core purposes and illustrating how each contributes to the broader practice of medicine.
1. Internal Medicine
Internal medicine is the foundation of adult medical care. Internists specialize in diagnosing, treating, and preventing diseases that affect adults, particularly complex or chronic conditions. Their work spans multiple organ systems, requiring a broad understanding of physiology and pathology. Internists often serve as primary care physicians, coordinating care among subspecialists and managing long‑term health issues such as hypertension, diabetes, and heart disease.
2. Family Medicine
Family medicine emphasizes comprehensive, continuous care for individuals and families across all ages, genders, and health conditions. Unlike internal medicine, which focuses on adults, family physicians treat children, adolescents, adults, and older adults. Their holistic approach integrates preventive care, acute illness management, and chronic disease monitoring. Family medicine values long‑term relationships and community‑based practice.
3. Pediatrics
Pediatrics is dedicated to the health of infants, children, and adolescents. Pediatricians address developmental milestones, childhood illnesses, congenital disorders, and preventive care such as vaccinations. They must understand not only the physiology of growing bodies but also the emotional and social needs of young patients. Pediatricians often collaborate closely with families to support healthy development.
4. Obstetrics and Gynecology (OB/GYN)
OB/GYN combines two related fields: obstetrics, which focuses on pregnancy, childbirth, and postpartum care, and gynecology, which addresses the health of the female reproductive system. Specialists in this field manage prenatal care, deliver babies, perform reproductive surgeries, and treat conditions such as endometriosis, infertility, and menstrual disorders. OB/GYN physicians balance surgical skill with long‑term patient care.
5. Surgery
Surgery is one of the oldest and most technically demanding medical specialties. Surgeons diagnose and treat diseases, injuries, and deformities through operative procedures. General surgeons handle a wide range of abdominal, breast, and soft‑tissue conditions, while many pursue subspecialties such as vascular, colorectal, or trauma surgery. Surgical practice requires precision, decisiveness, and the ability to manage perioperative care.
6. Orthopedic Surgery
Orthopedic surgery focuses on the musculoskeletal system, including bones, joints, ligaments, tendons, and muscles. Orthopedic surgeons treat fractures, sports injuries, degenerative diseases like arthritis, and congenital deformities. Their work often involves reconstructive procedures, joint replacements, and minimally invasive techniques. This specialty blends mechanical understanding with surgical expertise.
7. Cardiology
Cardiology is the study and treatment of diseases of the heart and blood vessels. Cardiologists manage conditions such as coronary artery disease, arrhythmias, heart failure, and hypertension. They use diagnostic tools like electrocardiograms, echocardiograms, and stress tests to evaluate cardiovascular function. Some cardiologists specialize further in interventional procedures, electrophysiology, or advanced heart failure management.
8. Neurology
Neurology focuses on disorders of the nervous system, including the brain, spinal cord, and peripheral nerves. Neurologists diagnose and treat conditions such as epilepsy, stroke, multiple sclerosis, migraines, and neurodegenerative diseases. Their work requires careful clinical examination and interpretation of imaging and electrophysiological tests. Neurology often intersects with psychiatry, rehabilitation, and neurosurgery.
9. Psychiatry
Psychiatry is the medical specialty devoted to mental, emotional, and behavioral health. Psychiatrists evaluate and treat conditions such as depression, anxiety disorders, bipolar disorder, schizophrenia, and substance‑related disorders. They use a combination of psychotherapy, behavioral interventions, and medication management. Psychiatry uniquely bridges biological and psychological perspectives on human health.
10. Dermatology
Dermatology addresses diseases of the skin, hair, and nails. Dermatologists diagnose and treat conditions such as eczema, psoriasis, acne, skin infections, and skin cancers. They perform procedures including biopsies, excisions, and cosmetic treatments. Because the skin reflects both internal and external influences, dermatologists often collaborate with other specialists to identify systemic causes of dermatologic symptoms.
***
***
11. Ophthalmology
Ophthalmology is the medical and surgical care of the eyes and visual system. Ophthalmologists treat conditions such as cataracts, glaucoma, macular degeneration, and retinal disorders. They perform delicate microsurgeries and use advanced imaging to assess ocular health. Vision is central to daily life, making ophthalmology essential for preserving quality of life.
12. Otolaryngology (ENT)
Otolaryngology—often called ENT—focuses on disorders of the ear, nose, throat, head, and neck. ENT specialists treat hearing loss, sinus disease, voice disorders, sleep apnea, and head‑and‑neck cancers. Their work includes both medical management and surgical procedures, ranging from tonsillectomies to complex reconstructive surgeries.
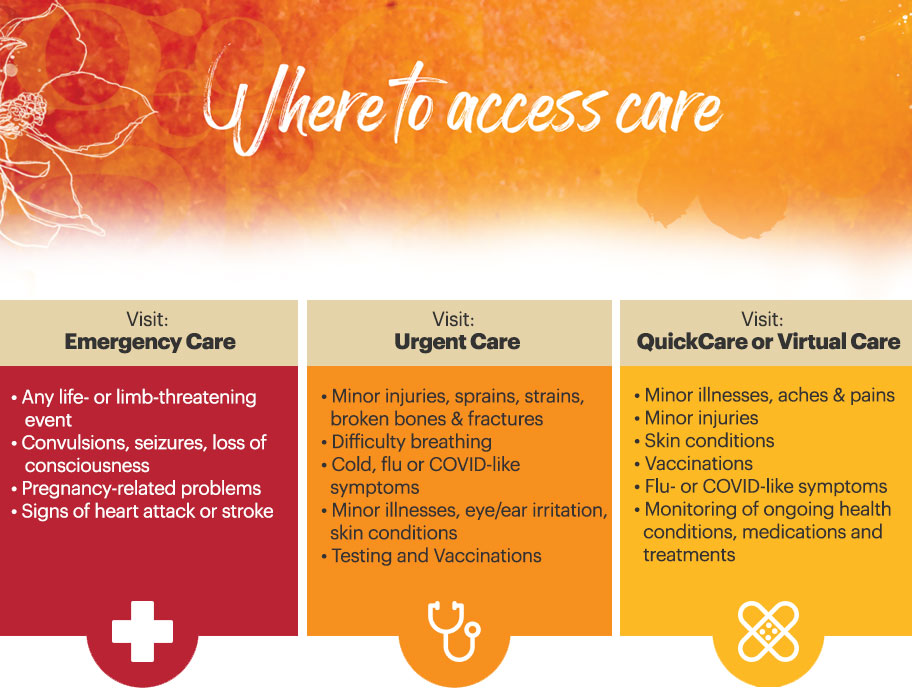
13. Emergency Medicine
Emergency medicine physicians provide immediate care for acute illnesses and injuries. They work in fast‑paced environments where rapid assessment and stabilization are critical. Emergency physicians treat trauma, heart attacks, strokes, infections, and a wide range of urgent conditions. Their broad training allows them to manage patients of all ages and coordinate care with specialists.
14. Anesthesiology
Anesthesiology centers on pain management and the safe administration of anesthesia during surgical and medical procedures. Anesthesiologists monitor vital functions, manage airway and breathing, and ensure patient comfort. They also provide critical care, acute pain services, and chronic pain management. Their role is essential for modern surgery and intensive care.
15. Radiology
Radiology involves the use of imaging technologies to diagnose and sometimes treat disease. Radiologists interpret X‑rays, CT scans, MRIs, ultrasounds, and nuclear medicine studies. Interventional radiologists perform minimally invasive procedures guided by imaging, such as angioplasty or tumor ablation. Radiology is central to accurate diagnosis across nearly all medical specialties.
16. Pathology
Pathology is the study of disease at the microscopic and molecular levels. Pathologists analyze tissue samples, blood, and bodily fluids to identify abnormalities and provide definitive diagnoses. Their work includes surgical pathology, cytology, and laboratory medicine. Although they often work behind the scenes, pathologists are essential for confirming diagnoses and guiding treatment decisions.
17. Oncology
Oncology focuses on the diagnosis and treatment of cancer. Oncologists manage chemotherapy, immunotherapy, targeted therapy, and palliative care. They work closely with surgeons, radiologists, and pathologists to develop comprehensive treatment plans. Oncology requires not only scientific expertise but also compassionate communication, as patients often face life‑altering diagnoses.
18. Endocrinology
Endocrinology addresses disorders of the endocrine system, which regulates hormones. Endocrinologists treat conditions such as diabetes, thyroid disease, adrenal disorders, and metabolic bone disease. Because hormones influence nearly every bodily function, endocrinologists must understand complex physiological interactions and long‑term disease management.
19. Gastroenterology
Gastroenterology focuses on the digestive system, including the esophagus, stomach, intestines, liver, pancreas, and gallbladder. Gastroenterologists diagnose and treat conditions such as inflammatory bowel disease, liver disease, ulcers, and gastrointestinal cancers. They perform endoscopic procedures to visualize and treat internal structures. Digestive health plays a crucial role in overall well‑being, making this specialty vital.
20. Nephrology
Nephrology is the study and treatment of kidney diseases. Nephrologists manage chronic kidney disease, electrolyte imbalances, hypertension related to kidney dysfunction, and dialysis care. They play a central role in preventing kidney failure and supporting patients who require renal replacement therapy. Because the kidneys influence many bodily systems, nephrology often overlaps with cardiology, endocrinology, and critical care.
Conclusion
The diversity of medical specialties reflects the complexity of human health. Each specialty contributes a unique perspective, set of skills, and body of knowledge, yet all share the common goal of improving patient well‑being. From the precision of surgery to the holistic approach of family medicine, from the microscopic focus of pathology to the emotional insight of psychiatry, these twenty specialties illustrate the breadth of modern medicine. Understanding them not only clarifies how healthcare is organized but also highlights the collaborative nature of caring for patients in an increasingly specialized world.
COMMENTS APPRECIATED
SPEAKING: Dr. Marcinko will be speaking and lecturing, signing and opining, teaching and preaching, storming and performing at many locations throughout the USA this year! His tour of witty and serious pontifications may be scheduled on a planned or ad-hoc basis; for public or private meetings and gatherings; formally, informally, or over lunch or dinner. All medical societies, financial advisory firms or Broker-Dealers are encouraged to submit an RFP for speaking engagements: CONTACT: Ann Miller RN MHA at MarcinkoAdvisors@outlook.com -OR- http://www.MarcinkoAssociates.com
Like, Refer and Subscribe
***
***
Filed under: Ask a Doctor, Career Development, Glossary Terms, Health Law & Policy, Touring with Marcinko | Tagged: anesthesiology, cardiology, david marcinko, dermatology, ENT, GI, GYN, health, healthcare, nephrology, neurology, OB, Oncology, opthalmology, pathology, pediatrics, psychiatry, pulmonology, radiology, S&P 500, surgery, wellness | Leave a comment »