Dr. David Edward Marcinko MBA MEd
SPONSOR: http://www.HealthDictionarySeries.org
***
***
P-4-P DEFINED
Pay‑for‑performance (P4P) has become one of the most widely discussed strategies for improving healthcare quality in modern health systems. At its core, P4P links financial incentives to specific measures of performance, such as patient outcomes, adherence to clinical guidelines, or efficiency metrics. The idea is straightforward: reward providers for delivering high‑quality care, and they will be more motivated to improve their practices. Yet the simplicity of the concept masks a complex set of challenges, trade‑offs, and ethical considerations that shape how P4P functions in real‑world healthcare environments.
One of the primary arguments in favor of P4P is that it attempts to shift healthcare away from volume‑based reimbursement. Traditional fee‑for‑service models reward providers for doing more—more tests, more procedures, more visits—regardless of whether those services improve patient health. P4P, in contrast, aims to reward value rather than volume. By tying payment to outcomes or evidence‑based processes, the model encourages clinicians to focus on preventive care, chronic disease management, and coordination across the continuum of care. In theory, this alignment of financial incentives with patient well‑being should lead to better outcomes and more efficient use of resources.
***
***
Another potential benefit of P4P is its ability to promote transparency and accountability. When performance metrics are clearly defined and publicly reported, providers have a clearer understanding of expectations and benchmarks. This can foster a culture of continuous improvement, where clinicians and organizations regularly evaluate their performance and identify opportunities for better care. For patients, transparency can empower more informed decision‑making and build trust in the healthcare system.
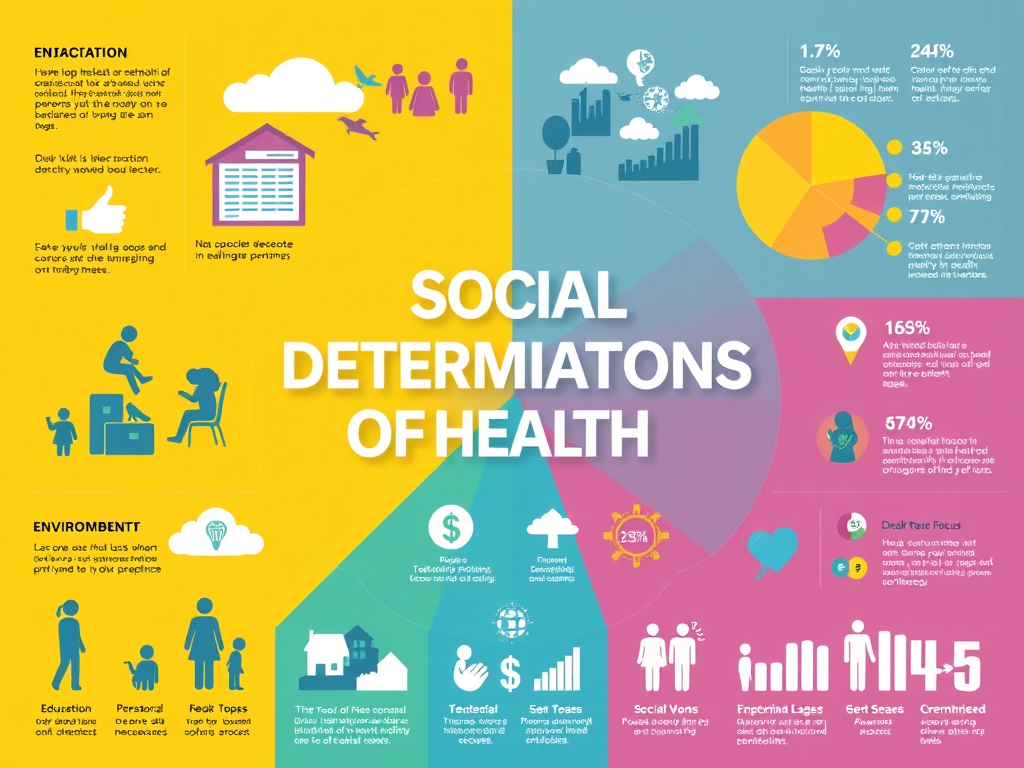
Despite these advantages, P4P is far from a perfect solution. One of the most persistent criticisms is that performance metrics often fail to capture the full complexity of patient care. Healthcare outcomes are influenced by a wide range of factors, many of which lie outside a provider’s control, such as socioeconomic conditions, patient adherence, and comorbidities. When incentives are tied to outcomes without adequate risk adjustment, providers may be unfairly penalized for caring for more complex or disadvantaged populations. This can inadvertently discourage clinicians from accepting high‑risk patients, undermining equity in access to care.
Another challenge is the potential for P4P to encourage “teaching to the test.” When financial rewards depend on specific metrics, providers may focus narrowly on those measures at the expense of other important aspects of care that are harder to quantify. This can lead to a checkbox mentality, where meeting the metric becomes more important than understanding the patient’s broader needs. In extreme cases, P4P can even incentivize gaming the system, such as upcoding diagnoses to make patient populations appear sicker and performance outcomes appear better.
Implementation complexity also poses a barrier. Designing fair, meaningful, and comprehensive performance measures requires significant administrative effort. Providers must invest time and resources into documentation, data reporting, and quality improvement initiatives. Smaller practices, which often lack the infrastructure of large health systems, may struggle to keep up with these demands. If the administrative burden outweighs the financial incentives, P4P can become more of a bureaucratic hurdle than a driver of improvement.
***
***
Ultimately, the effectiveness of pay‑for‑performance depends on thoughtful design and careful balancing of incentives. When metrics are clinically meaningful, risk‑adjusted, and aligned with broader goals of patient‑centered care, P4P can encourage positive change. When poorly designed, it risks distorting provider behavior and exacerbating inequities. As healthcare systems continue to evolve, P4P will likely remain part of the conversation, but it must be integrated with other reforms—such as care coordination models, population health strategies, and patient engagement efforts—to truly enhance quality and value.
COMMENTS APPRECIATED
SPEAKING: Dr. Marcinko will be speaking and lecturing, signing and opining, teaching and preaching, storming and performing at many locations throughout the USA this year! His tour of witty and serious pontifications may be scheduled on a planned or ad-hoc basis; for public or private meetings and gatherings; formally, informally, or over lunch or dinner. All medical societies, financial advisory firms or Broker-Dealers are encouraged to submit an RFP for speaking engagements: CONTACT: Ann Miller RN MHA at MarcinkoAdvisors@outlook.com -OR- http://www.MarcinkoAssociates.com
Like, Refer and Subscribe
***
***
Filed under: "Doctors Only", Ask a Doctor, Glossary Terms, Health Economics, Health Insurance, Health Law & Policy, Healthcare Finance, Touring with Marcinko | Tagged: david marcinko, Health Insurance, Healthcare Finance, Medical Pay‑for‑Performance, P-4-P, P4P | Leave a comment »