CYBER MONDAY
By Ann Miller RN MHA CPHQ
***
***
David Edward Marcinko’s Hospitals and Healthcare Organizations is a comprehensive exploration of the complex systems that underpin modern healthcare delivery. The book serves as both a practical guide and a conceptual framework for understanding how hospitals and related institutions function within the broader healthcare ecosystem. Marcinko’s work is notable for its ability to bridge the gap between theory and practice, offering readers insights into management, policy, finance, and patient care, all while emphasizing the interconnectedness of these domains.
One of the central themes of the book is the evolution of hospitals from charitable institutions into sophisticated organizations that must balance clinical excellence with financial sustainability. Marcinko highlights how hospitals have transformed over time, adapting to advances in medical technology, shifting patient expectations, and the pressures of regulatory oversight. This historical perspective is crucial because it underscores the dynamic nature of healthcare organizations, reminding readers that hospitals are not static entities but living systems that must continually evolve to meet societal needs.
The book also delves deeply into the organizational structures that define hospitals. Marcinko examines the roles of boards of directors, executive leadership, medical staff, and support personnel, illustrating how each group contributes to the overall mission of the institution. He emphasizes the importance of governance and accountability, noting that effective leadership is essential for aligning clinical priorities with financial realities. By presenting hospitals as multifaceted organizations, Marcinko encourages readers to appreciate the delicate balance required to maintain operational efficiency while delivering high‑quality patient care.
Another significant focus of the text is healthcare finance. Marcinko provides detailed discussions of reimbursement models, cost control strategies, and the economic challenges facing hospitals in an era of rising expenses and constrained resources. He explains how hospitals must navigate complex payment systems, including private insurance, government programs, and patient billing, while simultaneously investing in infrastructure and innovation. This financial lens is critical because it reveals the tension between the altruistic mission of healthcare and the pragmatic necessity of fiscal responsibility. Marcinko’s analysis makes clear that without sound financial management, even the most clinically advanced hospital cannot sustain itself.
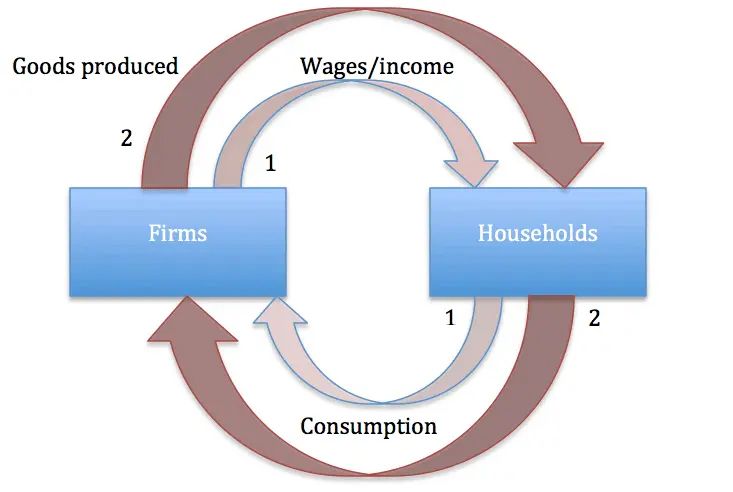
The book also addresses the role of hospitals within the larger healthcare delivery system. Marcinko situates hospitals alongside outpatient clinics, long‑term care facilities, and community health organizations, demonstrating how these entities form an integrated network of care. He argues that hospitals must collaborate with other providers to ensure continuity of care, reduce duplication of services, and improve patient outcomes. This systems‑based approach reflects the growing emphasis on coordinated care and population health management, both of which are essential for addressing the challenges of chronic disease and aging populations.
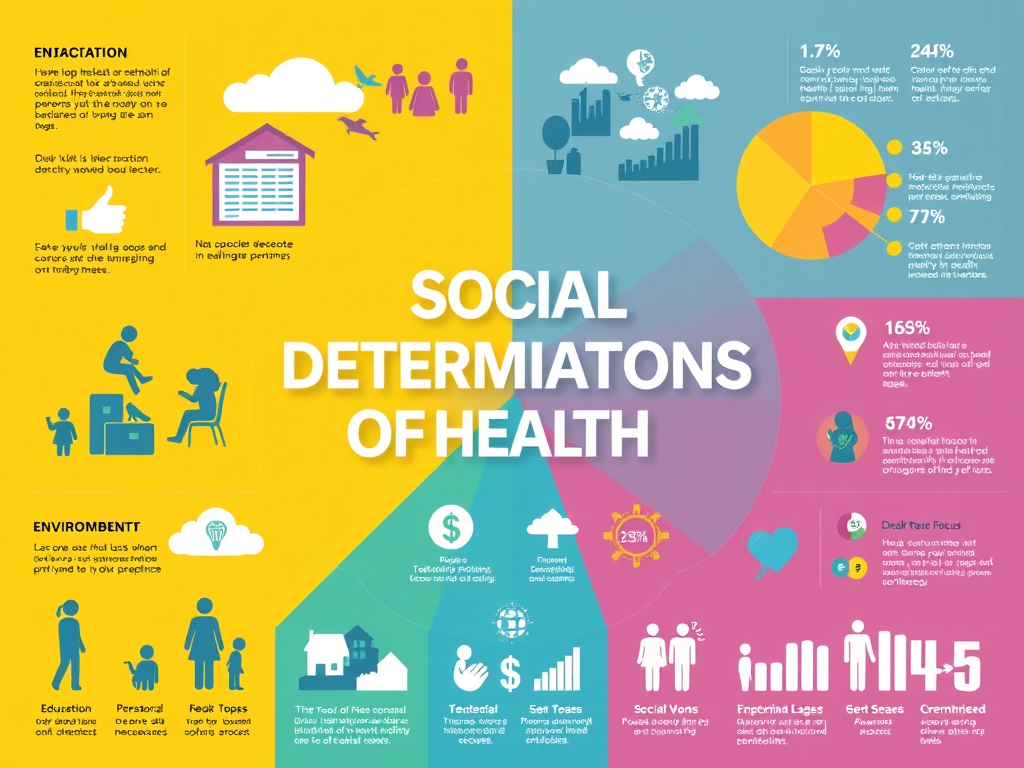
Marcinko does not shy away from discussing the ethical and social dimensions of hospital management. He explores issues such as access to care, disparities in health outcomes, and the responsibilities of hospitals to their communities. By weaving these considerations into his analysis, Marcinko reminds readers that hospitals are not merely businesses but social institutions with obligations that extend beyond their walls. This perspective reinforces the idea that healthcare organizations must balance profitability with compassion, efficiency with equity.
The book’s practical orientation is evident in its attention to strategic planning and operational improvement. Marcinko offers frameworks for decision‑making, performance measurement, and quality assurance, all of which are vital for hospital administrators and healthcare leaders. He stresses the importance of adaptability, urging organizations to remain responsive to external pressures such as policy changes, technological innovations, and shifting patient demographics. In doing so, he positions hospitals as dynamic entities that must constantly recalibrate their strategies to remain relevant and effective.
Ultimately, Hospitals and Healthcare Organizations is a valuable resource for anyone seeking to understand the complexities of healthcare management. Marcinko’s work combines historical context, organizational theory, financial analysis, and ethical reflection into a cohesive narrative that captures the multifaceted nature of hospitals. The book underscores the reality that hospitals are at once places of healing, centers of innovation, and businesses that must operate within competitive and regulated environments. By presenting hospitals in this holistic manner, Marcinko equips readers with the knowledge and perspective needed to navigate the challenges of modern healthcare.
In conclusion, Marcinko’s book is more than a manual for hospital administrators; it is a thoughtful examination of the role hospitals play in society. It highlights the delicate balance between clinical care and organizational sustainability, reminding readers that hospitals must serve both patients and communities while remaining financially viable. Through its blend of theory and practice, the book provides a roadmap for understanding and improving healthcare organizations in an ever‑changing landscape.
COMMENTS APPRECIATED
Like, Refer and Subscribe
***
***
Filed under: iMBA, Inc. | Tagged: AI, artificial intelligence, health, healthcare, Technology | Leave a comment »