Dr. David Edward Marcinko MBA MEd CMP
SPONSOR: http://www.CertifiedMedicalPlanner.org
***
***
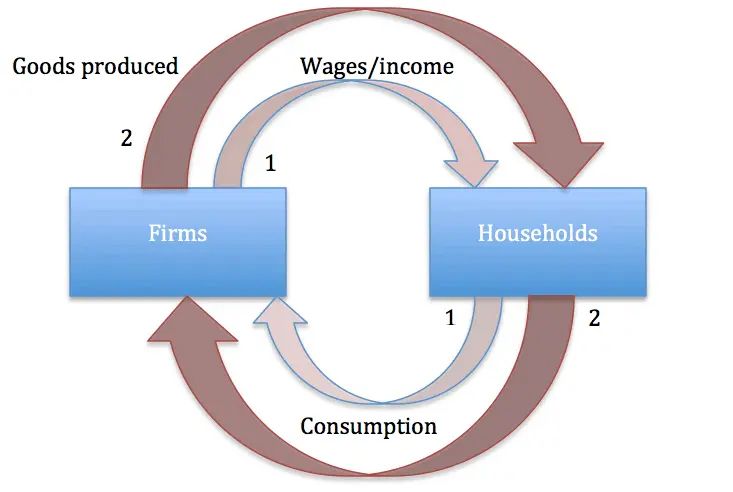
Financial fraud has long been woven into the fabric of American economic history. From Ponzi schemes to corporate deception, the United States has witnessed a series of high‑profile scandals that not only devastated investors but also reshaped regulatory frameworks. While the methods evolve with technology and time, the underlying motivations—greed, power, and the illusion of success—remain constant. This essay explores ten of the most notorious U.S. financial scammers whose actions left lasting scars on markets, institutions, and public trust.
1. Kenneth Lay & Jeffrey Skilling (Enron)
Few scandals loom as large as Enron, a company once hailed as an innovative energy titan before collapsing under the weight of its own deception. Enron executives Kenneth Lay and Jeffrey Skilling engineered an elaborate system of off‑balance‑sheet entities to hide debt and inflate earnings. The fraud, involving an estimated $74 billion, shattered investor confidence and triggered the Sarbanes‑Oxley Act, one of the most sweeping corporate governance reforms in U.S. history.
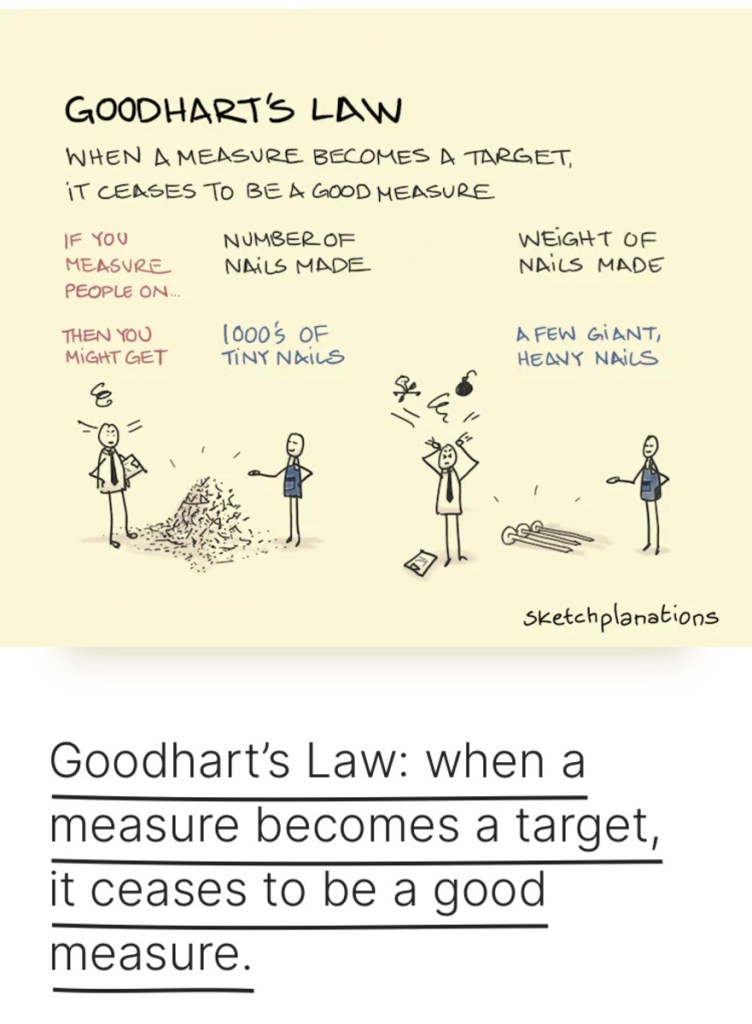
Their scheme demonstrated how corporate culture—when driven by unchecked ambition—can incentivize fraud at scale. Enron’s downfall remains a cautionary tale about transparency, oversight, and the dangers of financial engineering gone awry.
2. Bernie Madoff (Madoff Investment Securities)
Bernie Madoff orchestrated the largest Ponzi scheme in world history, defrauding investors of an estimated $65 billion. His reputation as a respected financier and former NASDAQ chairman allowed him to operate undetected for decades. Madoff’s scam unraveled during the 2008 financial crisis, exposing how trust, prestige, and secrecy can mask catastrophic fraud.
Though not directly cited in the retrieved sources, Madoff’s case is widely recognized as one of the most consequential financial crimes in U.S. history.
3. Andrew Fastow (Enron CFO)
While Lay and Skilling were the public faces of Enron, CFO Andrew Fastow was the architect behind the company’s labyrinth of special‑purpose vehicles (SPVs). These entities allowed Enron to hide massive liabilities while presenting a façade of profitability. Fastow personally profited from managing these off‑books partnerships, blurring the line between corporate officer and self‑interested operator. His actions exemplify how technical accounting knowledge can be weaponized to deceive investors.
4. Elizabeth Holmes (Theranos)
Elizabeth Holmes captivated Silicon Valley and Wall Street with promises of revolutionary blood‑testing technology. Theranos, valued at $9 billion at its peak, claimed it could run hundreds of tests from a single drop of blood. Investigations later revealed that the technology did not work, and the company relied on traditional machines while misleading investors, regulators, and patients.
Holmes’ downfall highlighted the dangers of hype‑driven investment culture and the need for scientific validation in health‑tech ventures.
5. Allen Stanford (Stanford Financial Group)
Allen Stanford ran a massive Ponzi scheme disguised as a global banking empire. Through fraudulent certificates of deposit issued by his Antigua‑based bank, Stanford defrauded investors of more than $7 billion. His charisma and lavish lifestyle helped him cultivate an image of legitimacy, masking the underlying fraud for years.
Stanford’s case underscored the vulnerabilities in cross‑border financial regulation and the risks of opaque offshore banking structures.
***
***
6. Jordan Belfort (Stratton Oakmont)
Popularized by The Wolf of Wall Street, Jordan Belfort’s pump‑and‑dump schemes in the 1990s defrauded investors through aggressive sales tactics and artificially inflated stock prices. While his crimes were smaller in scale than others on this list, Belfort’s cultural impact is enormous. His story illustrates how manipulation, high‑pressure sales, and market hype can devastate unsuspecting investors.
7. Charles Ponzi (The Original Ponzi Scheme)
Although his scheme dates back to the early 20th century, Charles Ponzi’s name remains synonymous with financial fraud. His promise of extraordinary returns through international postal coupon arbitrage attracted thousands of investors. When the scheme collapsed, it revealed the classic structure of a fraud model still used today: paying old investors with new investors’ money.
Ponzi’s legacy endures as a blueprint for countless modern scams.
8. Martin Shkreli (Turing Pharmaceuticals)
Martin Shkreli, often dubbed “Pharma Bro,” became infamous for dramatically raising the price of a life‑saving drug. While his price‑gouging was legal, Shkreli was later convicted of securities fraud unrelated to the drug scandal. His case illustrates how unethical behavior in one domain can draw scrutiny that uncovers deeper financial misconduct.
***
***
9. Sam Bankman‑Fried (FTX)
Sam Bankman‑Fried’s cryptocurrency exchange FTX collapsed in 2022 amid revelations of misused customer funds, lack of internal controls, and deceptive financial practices. Although crypto is a new frontier, the underlying fraud echoed classic themes: commingled funds, misleading investors, and unchecked executive power.
Bankman‑Fried’s downfall signaled a turning point in calls for crypto regulation and transparency.
10. Modern Imposter & Digital Scammers
While not tied to a single individual, modern imposter scams represent one of the fastest‑growing categories of financial fraud in the U.S. According to the Federal Trade Commission, Americans lost $5.8 billion to fraud in a single reporting year, with imposter scams leading the list. These schemes often involve criminals posing as government officials, financial advisors, or tech support agents to extract money or personal information.
Digital fraudsters exploit urgency, fear, and technological sophistication to deceive victims. As noted in recent analyses, imposter scams remain among the most prevalent and damaging forms of financial deception today.
Conclusion
The stories of these ten financial scammers reveal recurring themes: the power of perceived legitimacy, the exploitation of trust, and the persistent evolution of fraudulent tactics. From Enron’s corporate labyrinth to Madoff’s quiet betrayal, from Silicon Valley hype to digital‑age imposters, financial fraud continues to adapt to new technologies and cultural shifts.
Yet each scandal also brings progress. Regulatory reforms, improved oversight, and increased public awareness have emerged from the wreckage of these schemes. Understanding the methods and motivations of past scammers is essential to preventing future ones. As long as financial systems exist, so too will those who seek to exploit them—but informed vigilance remains society’s strongest defense.
COMMENTS APPRECIATED
SPEAKING: Dr. Marcinko will be speaking and lecturing, signing and opining, teaching and preaching, storming and performing at many locations throughout the USA this year! His tour of witty and serious pontifications may be scheduled on a planned or ad-hoc basis; for public or private meetings and gatherings; formally, informally, or over lunch or dinner. All medical societies, financial advisory firms or Broker-Dealers are encouraged to submit an RFP for speaking engagements: CONTACT: Ann Miller RN MHA at MarcinkoAdvisors@outlook.com -OR- http://www.MarcinkoAssociates.com
Like, Refer and Subscribe
***
***
Filed under: CMP Program, economics, finance, Financial Planning, Funding Basics, Glossary Terms, Health Economics, Health Insurance, Health Law & Policy, Healthcare Finance, Investing, Touring with Marcinko | Tagged: Bankman-Fried, belfort, crypto scams, david marcinko, design, digital scams, fastow, financial scammers, Holmes, Jeff Skilling, Ken Lay, Madoff, marketing, open-source, ponzie, Science, shkreli, skilling, Stanford, Technology | Leave a comment »