Dr. David Edward Marcinko MBA MEd
***
***
Why podiatry surgery volume matters so much?
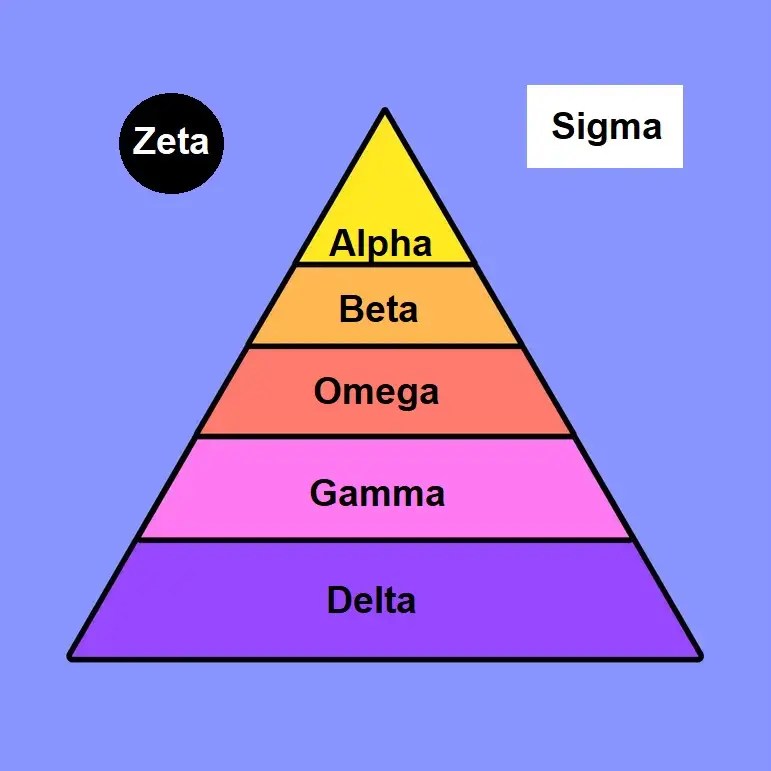
Podiatry Management Service Organizations typically rely on three revenue pillars:
- Office visits (high volume, low margin)
- Ancillaries (DME, orthotics, imaging)
- Surgery (low volume, high margin)
Surgery is the only pillar that reliably moves EBITDA in a meaningful way. Buyers know this, so they scrutinize surgical volume harder than anything else.
***
***
🔍 What “surgery volume” really means in podiatry
It’s not just the number of cases. Buyers look at:
- Case mix (forefoot vs. rearfoot vs. trauma)
- Site of service (ASC vs. hospital vs. office)
- Provider concentration (is one surgeon doing 40% of cases?)
- Payer mix (Medicare vs. commercial)
- Seasonality (podiatry has real seasonal swings)
- Referral stability (orthopedics, PCPs, wound care centers)
If any of these look unstable, the MSO’s valuation drops fast.
🚧 What happens to surgery volume when an MSO misses its exit window
1. Surgeons become less motivated
When the exit stalls:
- Equity feels less valuable
- Surgeons may slow down elective cases
- Some shift cases back to hospitals
- Others reduce ASC utilization
- A few may even explore leaving the MSO
This is one of the biggest hidden risks.
2. Case mix often deteriorates
High‑value cases (rearfoot, reconstructive, trauma) may decline, while:
- Nail procedures
- Callus debridements
- Routine diabetic care
…take up more of the schedule. This drags down EBITDA even if total visit volume stays stable.
3. Referral patterns weaken
If the MSO is perceived as unstable:
- Orthopedic groups may stop referring
- PCPs may shift to independent podiatrists
- Wound care centers may diversify referrals
Referral leakage is subtle but devastating.
4. ASC strategy becomes strained
Many podiatry MSOs depend on:
- Owning ASCs
- Leasing block time
- Negotiating better payer rates
If surgery volume softens:
- ASC utilization drops
- Fixed costs become painful
- Lenders get nervous
- Buyers discount the valuation
ASC underperformance is one of the top reasons podiatry MSOs fail to exit.
5. Productivity gaps widen between providers
Podiatry MSOs often have:
- A few high‑volume surgeons
- Many low‑volume generalists
When the exit stalls:
- High performers may feel under‑rewarded
- Low performers may drag down averages
- Buyers see concentration risk
If one surgeon leaves, the MSO’s EBITDA can collapse.
6. Compliance scrutiny increases
Surgical coding in podiatry is a known risk area. When an MSO can’t sell, buyers often dig deeper into:
- Modifier usage
- Global period billing
- Site‑of‑service documentation
- Medical necessity for certain procedures
If anything looks aggressive, the deal dies.
***
***
🎯 The bottom line
Podiatry surgery volume is the core value driver of a podiatry MSO. When an MSO fails to sell at its vintage year, surgery volume usually:
- Softens
- Becomes more concentrated
- Shifts toward lower‑margin cases
- Shows referral instability
- Raises compliance questions
Buyers interpret this as EBITDA fragility, which is why podiatry MSOs often end up in continuation funds or sell at discounted multiples.
COMMENTS APPRECIATED
SPEAKING: Dr. Marcinko will be speaking and lecturing, signing and opining, teaching and preaching, storming and performing at many locations throughout the USA this year! His tour of witty and serious pontifications may be scheduled on a planned or ad-hoc basis; for public or private meetings and gatherings; formally, informally, or over lunch or dinner. All medical societies, financial advisory firms or Broker-Dealers are encouraged to submit an RFP for speaking engagements: CONTACT: Ann Miller RN MHA at MarcinkoAdvisors@outlook.com -OR- http://www.MarcinkoAssociates.com
Like, Refer and Subscribe
***
***
Filed under: "Ask-an-Advisor", "Doctors Only", Accounting, Ask a Doctor, economics, Experts Invited, finance, Financial Planning, Funding Basics, Glossary Terms, Health Economics, Investing, Touring with Marcinko | Tagged: david marcinko, Private Equity | Leave a comment »