By National Council on Disability
The origins of managed care can be traced back to at least 1929, when Michael Shadid, a physician in Elk City, Oklahoma, established a health cooperative for farmers in a small community without medical specialists or a nearby general hospital. He sold shares to raise money to establish a local hospital and created an annual fee schedule to cover the costs of providing care. By 1934, 600 family memberships were supporting a staff that included Dr. Shadid, four newly recruited specialists, and a dentist. That same year, two Los Angeles physicians, Donald Ross and Clifford Loos, entered into a prepaid contract to provide comprehensive health services to 2,000 employees of a local water company
Development of Prepaid Health Plans
Other major prepaid group practice plans were initiated between 1930 and 1960, including the Group Health Association in Washington, DC, in 1937, the Kaiser-Permanente Medical Program in 1942, the Health Cooperative of Puget Sound in Seattle in 1947, the Health Insurance Plan of Greater New York in New York City in 1947, and the Group Health Plan of Minneapolis in 1957. These plans encountered strong opposition from the medical establishment, but they also attracted a large number of enrollees.
Today, such prepaid health plans are commonly referred to as health maintenance organizations (HMOs). The term “health maintenance organization,” however, was not coined until 1970, with the aim of highlighting the importance that prepaid health plans assign to health promotion and prevention of illness. HMOs are what most Americans think of when the term “managed care” is used, even though other managed care models have emerged over the past 40 years.
Public Managed Care Plans
The enactment of the Health Maintenance Organization Act of 1973 (P. L. 93-222) provided a major impetus to the expansion of managed health care. The legislation was proposed by the Nixon Administration in an attempt to restrain the growth of health care costs and also to preempt efforts by congressional Democrats to enact a universal health care plan. P. L. 93-222 authorized $375 million to assist in establishing and expanding HMOs, overrode state laws restricting the establishment of prepaid health plans, and required employers with 25 or more employees to offer an HMO option if they furnished health insurance coverage to their workers. The purpose of the legislation was to stimulate greater competition within health care markets by developing outpatient alternatives to expensive hospital-based treatment. Passage of this legislation also marked an important turning point in the U.S. health care industry because it introduced the concept of for-profit health care corporations to an industry long dominated by a not-for-profit business model.
In the decade following the passage of P. L. 93-222, enrollment in HMOs grew slowly. Stiff opposition from the medical profession led to the imposition of regulatory restrictions on HMO operations. But the continued, rapid growth in health care outlays forced government officials to look for new solutions. National health expenditures grew as a proportion of the overall gross national product (GNP) from 5.3 percent in 1960 to 9.5 percent in 1980. In response, Congress in 1972 authorized Medicare payments to free-standing ambulatory care clinics providing kidney dialysis to beneficiaries with end-stage renal disease. Over the following decade, the Federal Government authorized payments for more than 2,400 Medicare procedures performed on an outpatient basis.
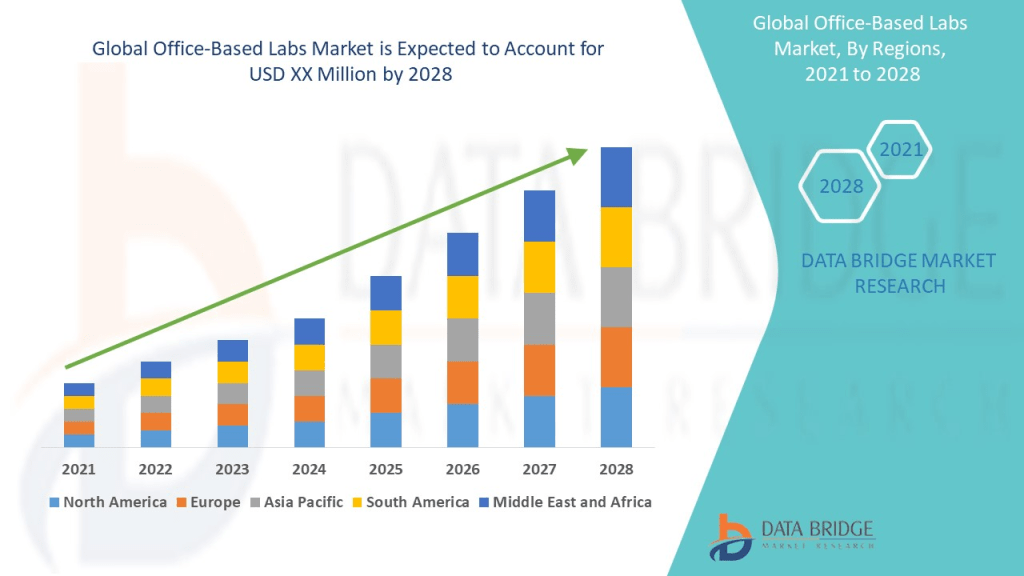
Responding to the relaxed regulatory environment, physicians began to form group practices and open outpatient centers specializing in diagnostic imaging, wellness and fitness, rehabilitation, surgery, birthing, and other services previously provided exclusively in hospital settings. As a result, the number of outpatient clinics skyrocketed from 200 in 1983 to more than 1,500 in 1991, and the percentage of surgeries performed in hospitals was halved between 1980 (83.7%) and 1992.

The Influence of Medicare Prospective Payments
Health care costs, however, continued to spiral upward, consuming 10.8 percent of GNP by 1983. In an attempt to slow the growth rate, Congress in 1982 capped hospital reimbursement rates under the Medicare program and directed the secretary of HHS to develop a case mix methodology for reimbursing hospitals based on diagnosis-related groups (DRGs). As an incentive to the hospital industry, the legislation (the Tax Equity and Fiscal Responsibility Act (P. L. 97-248)) included a provision allowing hospitals to avoid a Medicare spending cap by reaching an agreement with HHS on implementing a prospective payment system (PPS) to replace the existing FFS system. Following months of intense negotiations involving federal officials and representatives of the hospital industry, the Reagan Administration unveiled a Medicare PPS. Under the new system, health conditions were divided into 468 DRGs, with a fixed hospital payment rate assigned to each group.
Once the DRG system was fully phased in, Medicare payments to hospitals stabilized. However, since DRGs applied to inpatient hospital services only, many hospitals, like many group medical practices, began to expand their outpatient services in order to offset revenues lost as a result of shorter hospital stays. Between 1983 and 1991, the percentage of hospitals with outpatient care departments grew from 50 percent to 87 percent. Hospital revenues derived from outpatient services doubled over the period, reaching 25 percent of all revenues by 1992
Since DRGs were applied exclusively to Medicare payments, hospitals began to shift unreimbursed costs to private health insurance plans. As a result, average per employee health plan premiums doubled between 1984 and 1991, rising from $1,645 to $3,605. With health insurance costs eroding profits, many employers took aggressive steps to control health care expenditures. Plan benefits were reduced. Employees were required to pay a larger share of health insurance premiums. More and more employers—especially large corporations—decided to pay employee health costs directly rather than purchase health insurance. And a steadily increasing number of large and small businesses turned to managed health care plans in an attempt to rein in spiraling health care outlays.
Managed Long-Term Services and Supports
Arizona became the first state to apply managed care principles to the delivery and financing of Medicaid-funded LTSS in 1987, when the federal Health Care Financing Administration (later renamed the Centers for Medicare and Medicaid Services) approved the state’s request to expand its existing Medicaid managed care program. Medicaid recipients with physical and developmental disabilities became eligible to participate in the Arizona Long-Term Care System as a result of this program expansion. Over the following two decades, a number of other states joined Arizona in providing managed LTSS, and by the summer of 2012, 16 states were operating Medicaid managed LTSS programs
Growth of Commercial Managed Care Plans
During the late 1980s and early 1990s, managed care plans were credited with curtailing the runaway growth in health care costs. They achieved these efficiencies mainly by eliminating unnecessary hospitalizations and forcing participating physicians and other health care providers to offer their services at discounted rates. By 1993, a majority (51%) of Americans receiving health insurance through their employers were enrolled in managed health care plans. Eventually, however, benefit denials and disallowances of medically necessary services led to a public outcry and the enactment of laws in many states imposing managed care standards. According to one analysis, nearly 900 state laws governing managed health practices were enacted during the 1990s. Among the measures approved were laws permitting women to visit gynecologists and obstetricians without obtaining permission from their primary care physician, establishing the right of patients to receive emergency care, and establishing the right of patients to appeal decisions made by managed care firms. Congress even got into the act in 1997 when it passed the Newborns’ Mother Health Protection Act, prohibiting so-called “drive-through deliveries” (overly restrictive limits on hospital stays following the birth of a child).
Research studies have yielded little evidence that managed health care excesses have undermined the quality of health care services. For example, in a survey of 2,000 physicians, Remler and colleagues found that managed care insurance plans denied only about 1 percent of recommended hospitalizations, slightly more than 1 percent of recommended surgeries, and just over 2.5 percent of referrals to specialists. In another study, Franks and colleagues found that medical outcomes were similar for participants in HMOs versus FFS health plans. Franks also reported that HMO patients were hospitalized 40 percent less frequently than FFS patients, and the rate of inappropriate hospitalizations was lower among HMO patients.
Link: http://www.ncd.gov
More Recent Developments
Over the past 15 to 20 years, the public outcry against draconian managed care practices has waned, primarily due to the expanded out-of-network options afforded to participants in HMOs, PPOs, and POS health plans. But the perception that managed care represents an overly cost-conscious, mass market approach to delivering medical services lingers among the American public, even though more than 135 million people with health insurance coverage now receive their primary, preventive, and acute health services through a managed care plan. People with disabilities, especially high users of medical care and LTSS, share many of the same negative perceptions of managed care as the general public.
More:
Conclusion
Your thoughts and comments on this ME-P are appreciated. Feel free to review our top-left column, and top-right sidebar materials, links, URLs and related websites, too. Then, subscribe to the ME-P. It is fast, free and secure.
Speaker: If you need a moderator or speaker for an upcoming event, Dr. David E. Marcinko; MBA – Publisher-in-Chief of the Medical Executive-Post – is available for seminar or speaking engagements. Contact: MarcinkoAdvisors@msn.com
OUR OTHER PRINT BOOKS AND RELATED INFORMATION SOURCES:




Filed under: Experts Invited, Health Insurance, Managed Care, Op-Editorials, Practice Management | Tagged: ASC, History of Managed Care, Managed Care, National Council on Disability, NCD | 5 Comments »