By Dr. David Edward Marcinko MBA MEd CMP™
SPONSOR: http://www.CertifiedMedicalPlanner.org
***
***
What is a Paradox?
A paradox is a figure of speech that can seem silly or contradictory in form, yet it can still be true, or at least make sense in the context given. This is sometimes used to illustrate thoughts or statements that differ from traditional ideas. So, instead of taking a given statement literally, an individual must comprehend it from a different perspective. Using paradoxes in speeches and writings can also add wit and humor to one’s work, which serves as the perfect device to grab a reader or a listener’s attention.
But paradoxes can be quite difficult to explain by definition alone, which is why it is best to refer to a few examples to further your understanding.
A good paradox example is in the famous television show House. Here, Dr. House is a rude, selfish, and narcissistic character who alienates everyone around him, even his own colleagues. However, he is also a brilliant doctor who is committed to saving lives. Regardless of his mean exterior, Dr. House is a moral and compassionate man who cares about his patients. The paradox here is how the character strives to save people’s lives despite his ruthless personality and behavior.
Modern health care appears to be rich in contradictions, and it is claimed to be paradoxical in a number of ways. In particular health care is held to be a paradox itself: it is supposed to do good; but is also accused of doing harm.
- The expression “first do no harm,” which is a Latin phrase, is not part of the original or modern versions of the Hippocratic Oath, which was originally written in Greek (“primum non nocere,” the Latin translation from the original Greek.)
- The Hippocratic Oath, written in the 5th century BCE, does contain language suggesting that the physician and his assistants should not cause physical or moral harm to a patient.
- The first known published version of “do no harm” dates to medical texts from the mid-19th century, and is attributed to the 17th century English physician Thomas Sydenham.
Difference between Paradox and Oxymoron
Most people tend to confuse a paradox with an oxymoron, and it’s not hard to see why. Most oxymoron examples appear to be compressed version of a paradox, in which it is used to add a dramatic effect and to emphasize contrasting thoughts. Although they may seem greatly similar in form, there are slight differences that set them apart.
A paradox consists of a statement with opposing definitions, while an oxymoron combines two contradictory terms to form a new meaning. But because an oxymoron can play out with just two words, it is often used to describe a given object or idea imaginatively. As for a paradox, the statement itself makes you question whether something is true or false. It appears to contradict the truth, but if given a closer look, the truth is there but is merely implied.
The Paradox in Medicine and Health Care
Dr. Bernard Brom [Editor: SA Journal of Natural Medicine] suggests modem medicine is riddled with paradoxes. Most doctors live with these paradoxes without being aware of the conflict of interest that these paradoxes represent. Intrinsic to a general understanding of science is the idea that science frees us from misunderstanding and guides us towards clear decision making.
Most veteran doctors with experience know that medical science still does not give definitive answers, that each individual is unique, that one can never be sure how a patient will respond to a particular drug, or what the outcome of a particular operation will be. Human beings are not machines and therefore do not respond according to Newtonian logic, and therefore a paradox in medicine is not surprising. Medicine is an art which uses scientific techniques and approaches. It is, however, important to face these paradoxes. It is both humbling and enlightening, enriching those who consider the implications deeply enough.
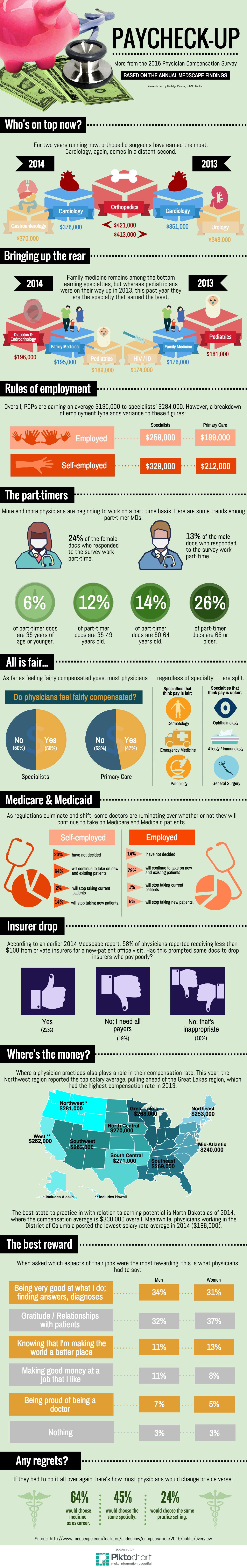
The Compensation versus Value Paradox
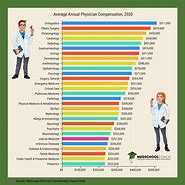
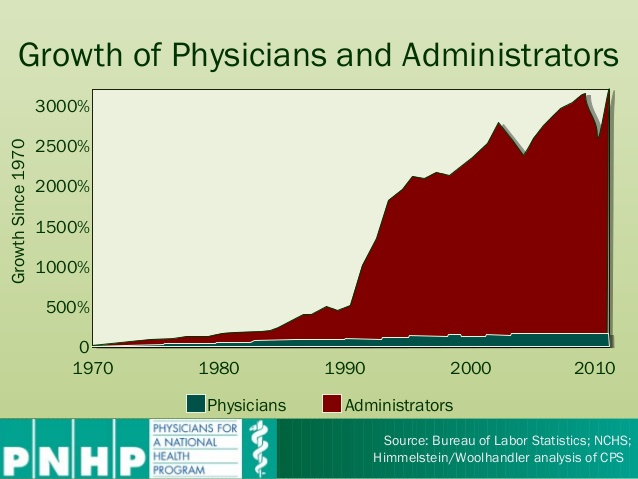
Regardless of specialty, degree designation or delivery model, private practice physician salary is traditionally inversely related to independent medical practice business value.
SALARY: https://medicalexecutivepost.com/2024/07/21/medicare-doctor-salary-rates-would-cut-pay-3/
In other words, the more a doctor takes home in compensation from his practice, the less ownership in a private practice is worth, and vice versa.
VALUE: https://medicalexecutivepost.com/2008/01/11/how-to-maximize-medical-practice-value/
Higher doctor salary equals lower practice appraisal value.
BROKE DOCTORS: https://medicalexecutivepost.com/2025/08/02/doctors-going-broke-and-living-paycheck-to-paycheck/
This is the difference between a short-term and long-term compensation strategy.
COMMENTS APPRECIATED
SPEAKING: Dr. Marcinko will be speaking and lecturing, signing and opining, teaching and preaching, storming and performing at many locations throughout the USA this year! His tour of witty and serious pontifications may be scheduled on a planned or ad-hoc basis; for public or private meetings and gatherings; formally, informally, or over lunch or dinner. All medical societies, financial advisory firms or Broker-Dealers are encouraged to submit an RFP for speaking engagements: CONTACT: Ann Miller RN MHA at MarcinkoAdvisors@outlook.com -OR- http://www.MarcinkoAssociates.com
Like and Subscribe
***
***
Filed under: "Advisors Only", Ask a Doctor, CMP Program, Drugs and Pharma, finance, Funding Basics, Healthcare Finance, Investing | Tagged: broke doctors, CMP, doctor compensation, medical practice ownership, paradox, physician compensation, physician salary, practice appraisals, practice value, private practice doctor, rick doctors, value paradox | Leave a comment »