Robert James Cimasi
Todd A. Zigrang
“Knowing is not enough; we must apply. Willing is not enough; we must do.” Goethe [1]
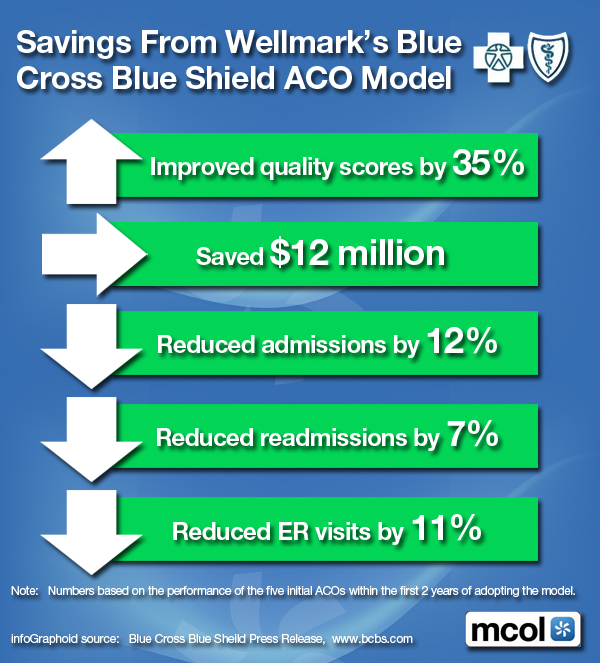
As developments in research and technology have advanced medical practice, the improved ability to diagnose and treat patients has led to an increased volume of medical assessments and procedures performed. However, these increases in the volume of procedures performed by physicians have led to an increase in both the risk of harm to patients and the exposure to liability for physicians.[2] Today, most healthcare services are delivered not by individual Marcus Welby type of physicians,[3] but through a group practice, healthcare organization, or hospital system. While there are numerous advantages to physicians providing care as employees of a healthcare enterprise, some of the unintended consequences exhibited under physician employment arrangements (e.g., diminishing physician autonomy, patient quotas, and limited time to spend with patients) have led to an increase in the potential for patient harm and subsequent physician liability.[4] Additionally, as the overlap between the scope of practice for physicians and non-physicians continues to increase, the complexities of malpractice liability, which may jeopardize the licenses of both the supervising physician and the non-physician professional, may similarly increase.[5] The result of these increased risks, medical errors, disgruntled patients, and changing scopes of practice has produced an environment that is ripe for malpractice litigation.[6]
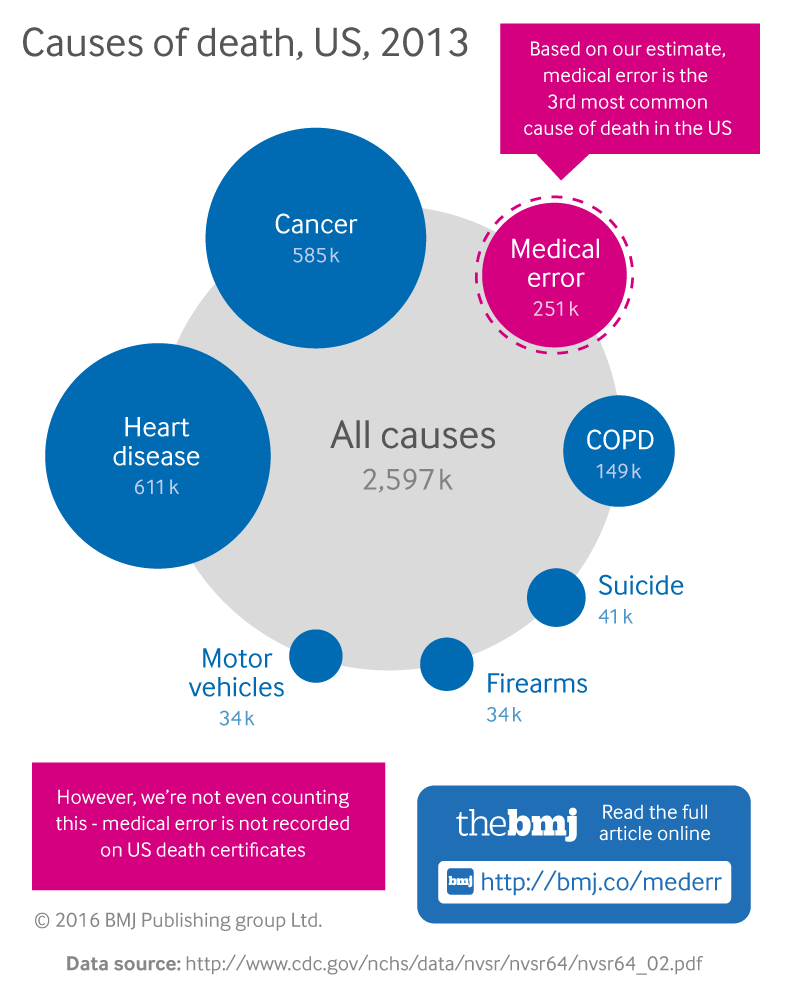
Numerous studies and examinations of the reality of medical errors demonstrate the varied nature and causes contributing to these errors, and the need for the medical malpractice system. The 2000 Institute of Medicine’s (IOM) landmark report, entitled, “To Err is Human: Building a Safer Health System,” conservatively estimated that in 1997, “at least 44,000 and perhaps as many as 98,000 Americans die in hospitals each year as a result of medical errors.”[7] Moreover, the IOM report noted that out of 30,000 discharges at 51 randomly selected New York hospitals in 1984, adverse events occurred in 3.7% of all hospitalizations or (1,110 hospitalizations), with 58% of adverse events (approximately 644 hospitalizations) caused by preventable medical errors, and 27.6% of adverse events (approximately 306 hospitalizations) caused by negligence.[8] In addition to medical errors, more than one million serious medication errors occur every year in U.S.[9] As observed in The Leapfrog Group’s study, one adverse drug effect (ADE) adds, on average, $2,000 to the cost of a hospitalization, which totals over $7.5 billion per year nationwide.[10]
Other studies have updated the figures relied upon in the IOM report. In 2010, the Office of Inspector General (OIG) estimated that approximately 13.5% of hospitalized Medicare beneficiaries experienced adverse events during their hospitalizations, 44% of which were deemed preventable by independent physician reviewers.[11] Within this estimate, the OIG subdivided the adverse events into four clinical categories:
- Events related to medication – 31%;
- Events related to ongoing patient care – 28%;
- Events related to surgery or other procedures – 26%; and,
- Events related to infection – 15%.[12]
A 2013 study published in Journal of Patient Safety combined the OIG’s estimate with the estimates of three other studies[13] relating to the prevalence of medical errors to conclude that over “210,000 preventable adverse events per year…contribute to the death of hospitalized patients,” with numerous additional errors shortening patients’ lifespans and causing other harms.[14]
The debate surrounding medical errors focuses not only on the number of adverse events in hospitals and deaths due to these adverse events, but also the causes of these adverse events. Although the 2000 IOM report is widely cited for its estimate of deaths due to medical errors,[15] the report also provided one of the first arguments that many medical errors “could likely have been avoided had better systems of care been in place,” framing the medical error debate not solely on “incompetent or impaired providers” but also on the process of care delivery.[16] These process improvements can center on infrastructure as well as policies and procedures regarding the provision of medical care. The same IOM committee that published the 2000 report released a second report in 2001 entitled, “Crossing the Quality Chasm: A New Health System for the 21st Century,” which advocated for widespread change in overall structures and processes in the healthcare environment as a means to preventing medical errors and improving quality, and listed six “aims” for high quality care: safety; effectiveness; efficiency; equity; timeliness; and, patient-centeredness.[17] However, a 2013 IOM report entitled, “Best Care at Lower Cost: The Path to Continuously Learning Health Care in America,” noted that, 12 years later, these six aims still had not been achieved, and attributed the “fragmented, uncoordinated, and diffusely organized” infrastructure of the U.S. healthcare delivery system to the lack of systemic processes in place.[18] Specifically addressing outpatient enterprise structures, a 2011 study on adverse drug events (ADEs) in ambulatory care settings noted the potential for infrastructure improvements to support the reduction of medical errors, stating that “as health information technology becomes more widespread in ambulatory health care delivery… automated surveillance for (adverse drug events) will become more feasible.”[19]
The OIG has provided similar guidance to healthcare providers regarding the relationship between structure and quality. In its revised guidance to nursing homes, the OIG recommended that nursing facilities can “promote compliance by having in place proper medication management processes,” such as utilizing a consultant pharmacist and continually training staff in proper medication management.[20] Nevertheless, criticism still exists regarding the processes utilized by healthcare providers to reduce medical errors. In its 2010 report on adverse events suffered by Medicare beneficiaries, the OIG recommended that the Centers for Medicare & Medicaid Services (CMS) “influence hospitals to reduce adverse events through enforcement of the conditions of participation” in Medicare, which includes sanctioning physicians through the peer review process.[21] Other studies have advanced the OIG’s claim a step further, arguing that “the hospital peer-review system has widespread failures that permit negligent care by physicians.”[22]
In an attempt “to improve patient safety by encouraging voluntary and confidential reporting of events that adversely affect patients,”[23] The Patient Safety and Quality Improvement Act (PSQIA) of 2005, effective January 19, 2009, established a voluntary reporting system for medical errors.[24] Under PSQIA, to address provider fear that “patient safety event reports could be used against them in medical malpractice cases or in disciplinary proceedings,”[25] confidentiality provisions regarding the protection of “patient safety work product” were established.[26] “Patient safety work product” includes any information that is collected while reporting and analyzing a patient safety event,[27] i.e., “a process or act of omission or commissions that resulted in hazardous health care conditions and/or unintended harm to the patient.”[28] Under PSQIA, Patient Safety Organizations (PSOs) are charged with collecting and analyzing data under the supervision of the Agency for Healthcare Research and Quality (AHRQ).[29]
Despite the numerous attempts and strategies to curtail the prevalence of medical errors, no definitive answer exists as to whether medical errors are properly attributable to process or physician errors on a large scale. If it were determined that most medical errors are mistakes from breakdowns in processes of care rather than the negligence of physicians, improving and implementing new and effective process controls may best reduce medical errors – and the resulting incidence of medical malpractice cases.[30] However, to date, the healthcare industry and the U.S. tort system are far from reaching this conclusion, leaving the tort system – as well as malpractice insurers and their physician insureds – to continue to grapple with this uncertainty.
[1] “Crossing the Quality Chasm: A New Health System for the 21st Century,” Institute of Medicine, National Academy of Sciences, 2001, front matter.
[2] “Overview of Medical Errors and Adverse Events,” By Maité Garrouste-Orgeas, et al., Annals of Intensive Care, Vol. 2, No. 2 (2012), p. 6.
[3] “Healthcare Valuation: The Financial Appraisal of Enterprises, Assets, and Services,” Vol. 1, By Robert James Cimasi, MHA, ASA, FRICS, CVA, CM&AA, Hoboken, NJ: John Wiley & Sons, 2014, p. xiii.
[4] “Health Law: Cases, Materials, and Problems, 7th Edition,” By Barry R. Furrow, Thomas L. Greaney, Sandra H. Johnson, Timothy Stoltzfus Jost, and Robert L. Schwartz, St. Paul, MN: West Publishing Company, 2013, p. 507.
[5] “Licensure of Health Care Professionals,” In “Health Care Law: A Practical Guide, Second Edition” By Scott Becker, Matthew Bender Co., 1998, § 16.02[4], p. 16-23.
[6] “Health Law: Cases, Materials, and Problems, 7th Edition,” By Barry R. Furrow, Thomas L. Greaney, Sandra H. Johnson, Timothy Stoltzfus Jost, and Robert L. Schwartz, St. Paul, MN: West Publishing Company, 2013, p. 506-507.
[7] “To Err is Human: Building a Safer Health System,” Institute of Medicine, National Academy of Sciences, 2000, p. 26. The IOM study extrapolated data from the 1984 New York study, as well as a 1992 study from Colorado and Utah to the number of hospitalizations in 1997 to estimate the number of deaths due to medical errors in 1997. The report authors note that these extrapolations may be low because the studies:
- “Considered only those patients whose injuries resulted in a specified level of harm;”
- “Imposed a high threshold to determine whether an adverse event was preventable or negligent;” and,
- “Included only errors that are documented in patient records.”
“To Err is Human: Building a Safer Health System,” Institute of Medicine, National Academy of Sciences, 2000, p. 31.
[8] “To Err is Human: Building a Safer Health System,” Institute of Medicine, National Academy of Sciences, 2000, p. 30.
[9] “Fact Sheet: Computerized Physician Order Entry,” The Leapfrog Group, March 3, 2009; “To Err is Human: Building a Safer Health System,” By Institute of Medicine, 2000, p.1.
[10] “Leapfrog Hospital Survey Results,” The Leapfrog Group, 2008, p. 3.
[11] “Adverse Events in Hospitals: National Incidence among Medicare Beneficiaries,” Office of Inspector General, November 2010, p. 15, 22.
[12] “Adverse Events in Hospitals: National Incidence among Medicare Beneficiaries,” Office of Inspector General, November 2010, p. 15.
[13] “‘Global Trigger Tool’ Shows That Adverse Events in Hospitals May be Ten Times Greater Than Previously Measured,” By David C. Classen et al., Health Affairs, Vol. 30, No. 4 (2011); “Adverse Events in Hospitals: Case Study of Incidence Among Medicare Beneficiaries in Two Selected Counties,” Office of Inspector General, December 2008, http://oig.hhs.gov/oei/reports/OEI-06-08-00220.pdf (Accessed 2/17/15); “Temporal Trends in Rates of Patient Harm Resulting from Medical Care” By Christopher P. Landrigan, MD, MPH, et al., New England Journal of Medicine, Vol. 363, No. 22 (November 24, 2010).
[14] “A New, Evidence-Based Estimate of Patient Harms Associated with Hospital Care” By John T. James, PhD, Journal of Patient Safety, Vol. 9. No. 3 (September 2013), p. 125.
[15] “How Many Die From Medical Mistakes in U.S. Hospitals?” By Marshall Allen, National Public Radio, September 20, 2013, http://www.npr.org/blogs/health/2013/09/20/224507654/howmanydiefrommedicalmistakesinushospitals (Accessed 12/3/14).
[16] “To Err is Human: Building a Safer Health System,” Institute of Medicine, National Academy of Sciences, 2000, p. 30.
[17] “Crossing the Quality Chasm: A New Health System for the 21st Century,” Institute of Medicine, National Academy of Sciences, 2001, p. ix, 25.
[18] “Best Care at Lower Cost: The Path to Continuously Learning Health Care in America,” Institute of Medicine, National Academy of Sciences, 2009, p. 134.
[19] “Adverse Drug Events in U.S. Adult Ambulatory Medical Care,” By Urmimala Sarkar et al., Health Services Research, Vol. 46, No. 5 (October 2011), p. 1527.
[20] “OIG Supplemental Compliance Program Guidance for Nursing Facilities,” Federal Register Vol. 73, No. 190 (September 30, 2008), p. 56837.
[21] “Adverse Events in Hospitals: National Incidence among Medicare Beneficiaries,” Office of Inspector General, November 2010, p. 32.
[22] “A New, Evidence-Based Estimate of Patient Harms Associated with Hospital Care”, By John T. James, PhD, Journal of Patient Safety, Vol. 9. No. 3 (September 2013), p. 127.
[23] “Patient Safety and Quality Improvement Act of 2005,” Agency for Healthcare Research and Quality, http://archive.ahrq.gov/news/newsroom/press-releases/2008/psoact.html (Accessed 3/5/15).
[24] “Health Information Privacy: Understanding Patient Safety Confidentiality,” U.S. Department of Health and Human Services, http://www.hhs.gov/ocr/privacy/psa/understanding/index.html (Accessed 3/5/15); “Patient Safety and Quality Improvement; Final Rule,” Federal Register, Vol. 73, No. 226 (November 21, 2008), p. 70732.
[25] “Patient Safety and Quality Improvement Act of 2005,” Agency for Healthcare Research and Quality, http://archive.ahrq.gov/news/newsroom/press-releases/2008/psoact.html (Accessed 3/5/15).
[26] “Patient Safety and Quality Improvement: Final Rule” Federal Register, Vol. 73, No. 226 (November 21, 2008), p. 70734.
[27] “Patient Safety and Quality Improvement: Final Rule” Federal Register, Vol. 73, No. 226 (November 21, 2008), p. 70739.
[28] “Patient Safety and Quality Improvement: Final Rule” Federal Register, Vol. 73, No. 226 (November 21, 2008), referring to footnote 7 in “Patient Safety and Quality Improvement: Proposed Rule” Federal Register, Vol. 73, No. 29 (February 12, 2008), p. 8113.
[29] “Understanding Patient Safety Confidentiality” U.S. Department of Health and Human Services, http://www.hhs.gov/ocr/privacy/psa/understanding/index.html (Accessed 3/5/15).
[30] “To Err is Human: Building a Safer Health System,” Institute of Medicine, National Academy of Sciences, 2000, p. 30.
Your thoughts are appreciated.
ORDER TEXTBOOK: https://www.routledge.com/Risk-Management-Liability-Insurance-and-Asset-Protection-Strategies-for/Marcinko-Hetico/p/book/9781498725989
THANK YOU
***
Filed under: iMBA, Inc. | Tagged: HCC, Health Capital Consultants LLC, malpractice, medical errorrs, robert james cimasi, Todd Zigrang | 2 Comments »





































 ***
***