By Dr. David Edward Marcinko MBA MEd
By Professor Eugene Schmuckler PhD MBA MEd CTS
***
***
Physician gambling addiction is a growing concern that threatens both personal well-being and professional integrity. This essay explores its causes, consequences, and the urgent need for awareness and support.
Gambling addiction, or gambling disorder, is a recognized mental health condition characterized by an uncontrollable urge to gamble despite negative consequences. While it affects about 1% of the general population., its presence among physicians is particularly alarming due to the high stakes involved—both financially and ethically. Physicians are entrusted with lives, and addiction can impair judgment, compromise patient care, and lead to devastating personal and professional outcomes.
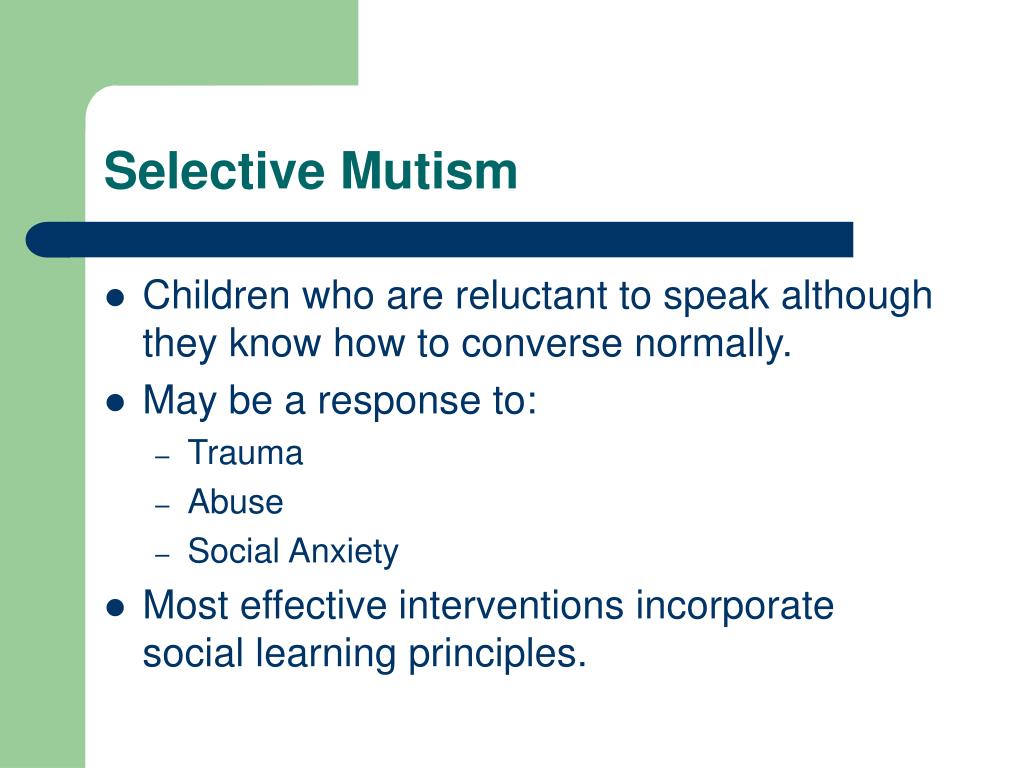
Several factors contribute to gambling addiction in physicians. The profession is inherently high-pressure, with long hours, emotional strain, and frequent exposure to trauma. These stressors can drive individuals to seek escape or excitement through gambling. Moreover, physicians often have access to substantial financial resources, making it easier to sustain gambling habits longer than others. The culture of perfectionism and stigma around mental health in medicine may also discourage seeking help, allowing addiction to fester in secrecy.
The consequences of gambling addiction for physicians are multifaceted. On a personal level, it can lead to financial ruin, strained relationships, and deteriorating mental health. Studies show that gambling activates the brain’s reward system similarly to drugs and alcohol, reinforcing compulsive behavior.
Professionally, addiction can result in medical errors, fraud, or even criminal activity—such as embezzling funds to cover gambling debts. These actions not only endanger patients but also erode public trust in the medical profession.
During the COVID-19 pandemic, gambling behavior intensified across many demographics, including healthcare workers. Increased isolation, stress, and access to online gambling platforms contributed to a surge in addiction cases. Physicians, already burdened by the pandemic’s demands, were particularly vulnerable. The rise of sports betting and fantasy leagues has further blurred the lines between entertainment and addiction, making it harder to recognize problematic behavior.
***
***
Addressing physician gambling addiction requires a multifaceted approach. First, medical institutions must foster a culture that encourages mental health support without stigma. Confidential counseling services, peer support groups, and educational programs can help physicians recognize and address addiction early. Licensing boards and hospitals should implement policies that balance accountability with rehabilitation, ensuring that affected physicians receive treatment rather than punishment alone.
Additionally, research into gambling disorder must continue to evolve. Institutions like Yale Medicine are leading efforts to understand the neurological and genetic underpinnings of addiction, which could inform more effective treatments. Public awareness campaigns can also help destigmatize gambling addiction and promote responsible behavior.
In conclusion, physician gambling addiction is a hidden crisis with far-reaching implications. It stems from a complex interplay of stress, access, and stigma, and its consequences can be catastrophic.
By promoting awareness, support, and research, the medical community can better protect its members and the patients they serve.
COMMENTS APPRECIATION
Like, Refer and Subscribe
***
***
Filed under: "Doctors Only", Ask a Doctor, Ethics, Health Insurance, Health Law & Policy, Healthcare Finance, LifeStyle, mental health | Tagged: anxiety, casino, depression, gambling addictions, gambling dds, gambling disoirder, gambling do, gambling doctors, gambling dpm, gambling md, gambling physicians, health, mental health, trauma | Leave a comment »