Enter the Weekendalists and Laborists
[By Dr. David Edward Marcinko; MBA]
Publisher-in-Chief
 More than a decade ago, in another career, I wrote a few articles for Richard L. Reece MD when he edited a print and emerging electronic trade publication for medical professionals. All very “fly”, at the time.
More than a decade ago, in another career, I wrote a few articles for Richard L. Reece MD when he edited a print and emerging electronic trade publication for medical professionals. All very “fly”, at the time.
The Laborists
Now – according to Dr. Reece who cites the Boston Globe, in “The Birth of a Notion”, a Cape Cod and some other Massachusetts hospitals are hiring “laborists”; aka board-certified obstetricians to work regular shifts for the sole purpose of delivering babies.
www.MedicalBusinessAdvisors.com
New Causitive Drivers
What drives these new-wave specialists? The answer, of course, is the next-generation of physicians and their emerging new medical business and practice models. Much like my 12 year old daughter, it is a way of professionally breaking away from past generations, and asserting some independence and leadership. And, as Martha Stewart might say; “that’s a good thing.”
Many Reasons
But, according to Reece, the real drivers are a combination of other things – the desire of doctors for regular hours, the shortage of specialists, physician burnout, the search for a safer hospital environment, the need for consistent, immediately available physician services, fear of dreaded malpractice suits, and consolidation of hospital-physicians services due to regulatory and economic pressures; etc.
Blended Generations
Dick is correct, of course, because it is not uncommon today to have three generations represented in healthcare. We have the Baby-boomers, Gen X and now, Gen Y. The Baby Boomer generation is saying with some sense of sadness that, “Medicine sure isn’t want it used to be!”, while Generation Xers are saying “It’s about time things changed!”, and the latest generation to enter the medical workforce, Gen Y’s, are saying “Ready or not, we’re here”.
http://www.BusinessofMedicalPractice.com
The Leadership Evolution
Each generation is extraordinarily complex, bringing various skills, expertise and expectations to the modern medical work environment. Determining the best method to unite such diverse thinking is one of the many challenges faced by physician executives and healthcare leaders. Is it any wonder that many medical leaders and executive in the Baby Boomer generation find themselves at a loss? The days of functional leadership are gone and suddenly, no one cares about the expertise of the Baby Boomers or how they climbed the corporate ladder, in medicine or elsewhere. Leadership in the era of Health 2.0 is no longer about command-control or dictating with intense focus on the bottom line; it is about collaboration, empowerment and communication. And, it is not about titles and nomenclature.
 Linguistic Evolution
Linguistic Evolution
As the linguistic evolution of terms progresses, the nomenclature of hospitalist was followed by that of intensivist, proceduralist, nocturalists, in-situ physician and even weekendalists. Think I’m kidding?
Link: http://medinnovationblog.blogspot.com/2009/02/hospital-based-doctorists.html
Assessment
I still like the causative analogy of my pre-teen daughter; it’s much simpler to understand. What do you think?
References
1. Wachter, R and Goldman, R: “The Emerging Role of ‘Hospitalists’ in the American Health System’. In, New England Journal of Medicine; 335, 514-517, 1996
2. Kowalczyk, L: The Birth of a Notion: Hospitals Turning to Laborarists. Boston Globe, February 23, 2009
Conclusion
Your thoughts and comments on this ME-P are appreciated. Feel free to review our top-left column, and top-right sidebar materials, links, URLs and related websites, too. Then, subscribe to the ME-P. It is fast, free and secure.
Speaker: If you need a moderator or speaker for an upcoming event, Dr. David E. Marcinko; MBA – Publisher-in-Chief of the Medical Executive-Post – is available for seminar or speaking engagements. Contact: MarcinkoAdvisors@msn.com
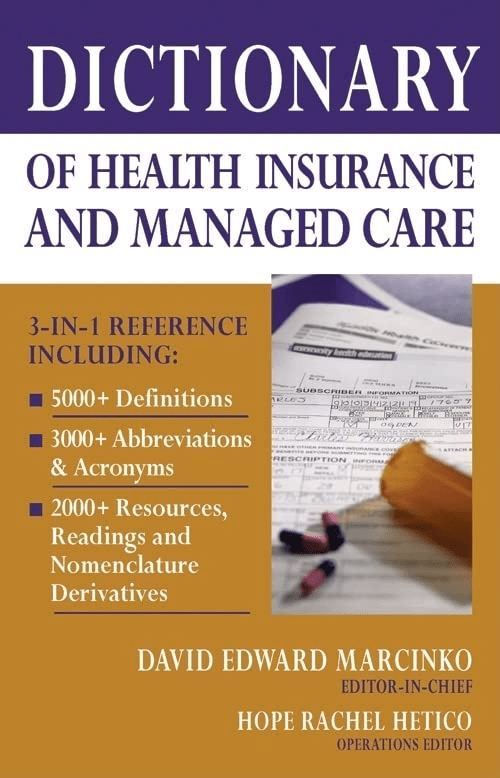
OUR OTHER PRINT BOOKS AND RELATED INFORMATION SOURCES:
***
[PHYSICIAN FOCUSED FINANCIAL PLANNING AND RISK MANAGEMENT COMPANION TEXTBOOK SET]


[Dr. Cappiello PhD MBA] *** [Foreword Dr. Krieger MD MBA]
***
Filed under: Career Development, iMBA, Inc. | Tagged: david marcinko, hospital medicine, hospitalists, hospitals, in-situ physician, intensivist, Marth Stewart, nocturalists, proceduralist, Richard L. Reece, rural hospitals, weekendalists | 2 Comments »