Origins of Diagnostic Related Groups
By Dr. David Edward Marcinko; MBA, CMP™
[Editor-in-Chief]
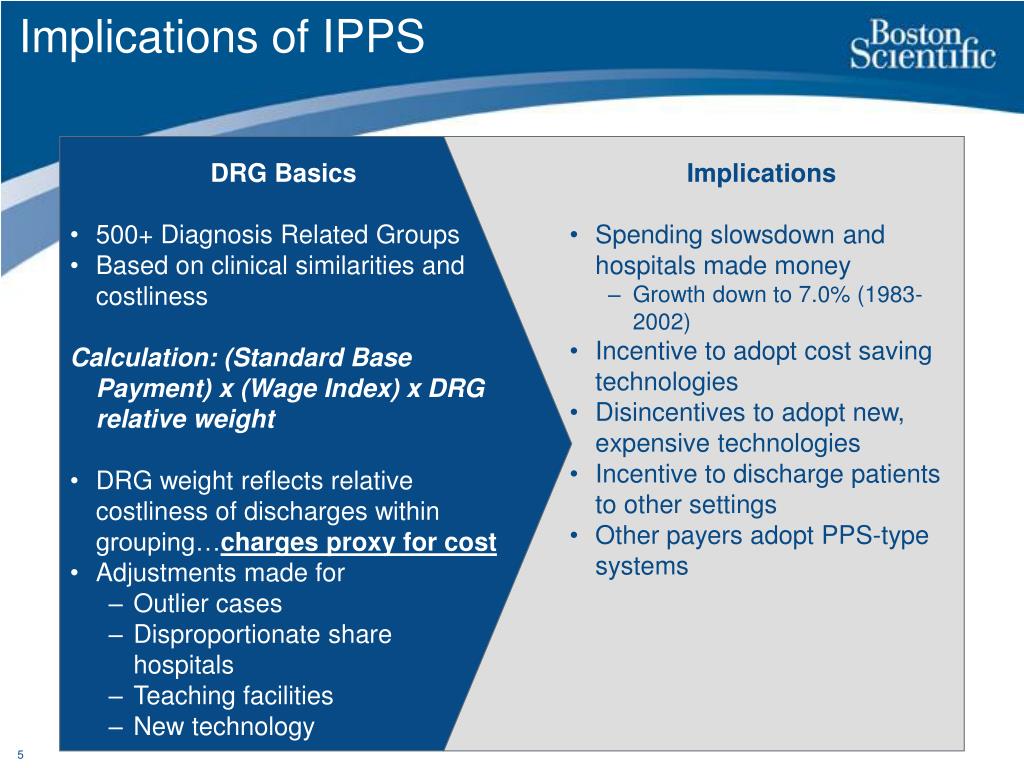
The Medicare Prospective Payment System (PPS) was introduced by the federal government in October, 1 1983, as a way to change hospital behavior through financial incentives that encourage more cost-efficient management of medical care. Under PPS, hospitals are paid a pre-determined rate for each Medicare admission. Each patient was classified into a diagnosis-related group (DRG) on the basis of clinical information. Except for certain patients with exceptionally high costs (“outliers”), the hospital is paid a flat rate for the DRG, regardless of the actual services provided.
Enter the DRGs
Each Medicare patient is classified into a DRG according to information from the medical record that appears on the bill:
- principal diagnosis (why the patient was admitted);
- complications and co-morbidities (other secondary diagnoses);
- surgical procedures;
- age and patient gender; and
- discharge disposition (routine, transferred, or expired).
Medical Records Documentation
Diagnoses and procedures must be documented by the attending physician in the patient’s medical record. They are then coded by hospital personnel using ICD-9-CM nomenclature. This is a numerical coding scheme of over 13,000 diagnoses and more than 5,000 procedures. The coding process is extremely important since it essentially determines what DRG will be assigned for a patient. Coding an incorrect principal diagnosis or failing to code a significant secondary diagnosis can dramatically affect reimbursement.
DRG Categories
Originally, there were more than 490 DRG categories defined by the Centers for Medicare and Medicaid Services (CMS, formerly known as the Health Care Financing Administration [HCFA]). Each category was designed to be “clinically coherent.” In other words, all patients assigned to a DRG are deemed to have a similar clinical condition. The PPS is based on paying the average cost for treating patients in the same DRG. Each year CMS makes technical adjustments to the DRG classification system that incorporates new technologies (e.g., laparoscopic procedures) and refines its use as a payment methodology. CMS also initiates changes to the ICD-9-CM coding scheme. The DRG assignment process is computerized in a program called the “grouper” that is used by hospitals and fiscal intermediaries. It was last significantly updated by CMS in 2006.
Assessment
Each year CMS also assigns a relative weight to each DRG. These weights indicate the relative costs for treating patients during the prior year. The national average charge for each DRG is compared to the overall average. This ratio is published annually in the Federal Register for each DRG. A DRG with a weight of 2.0000, for example, means that charges were historically twice the average; a DRG with a weight of 0.5000 was half the average; and so on.
Conclusion
Your thoughts and comments on this ME-P are appreciated. Feel free to review our top-left column, and top-right sidebar materials, links, URLs and related websites, too. Then, subscribe to the ME-P. It is fast, free and secure.
Link: http://feeds.feedburner.com/HealthcareFinancialsthePostForcxos
Speaker: If you need a moderator or speaker for an upcoming event, Dr. David E. Marcinko; MBA – Publisher-in-Chief of the Medical Executive-Post – is available for seminar or speaking engagements. Contact: MarcinkoAdvisors@msn.com
OUR OTHER PRINT BOOKS AND RELATED INFORMATION SOURCES:
LEXICONS: http://www.springerpub.com/Search/marcinko
PHYSICIANS: www.MedicalBusinessAdvisors.com
PRACTICES: www.BusinessofMedicalPractice.com
HOSPITALS: http://www.crcpress.com/product/isbn/9781466558731
CLINICS: http://www.crcpress.com/product/isbn/9781439879900
ADVISORS: www.CertifiedMedicalPlanner.org
BLOG: www.MedicalExecutivePost.com





Filed under: Health Economics, Health Insurance, Healthcare Finance, Practice Management | Tagged: Centers for Medicare and Medicaid Services, CMS, david marcinko, diagnosis-related group, DRG, HCFA, ICD-10-CM, ICD-9-CM, medicare, Medicare Prospective Payment System, PPS | 7 Comments »