Augmentation thru Technology Adoption
[By Karen White PhD, and Staff ]
Several major hospitals, or healthcare systems, have filed bankruptcy this fiscal quarter. These include a two-hospital system in Honolulu; one in Pontiac, MI; Trinity Hospital in Erin, Tennessee; Century City Doctors Hospital in Beverly Hills, and four hospital system Hospital Partners of America, in Charlotte.
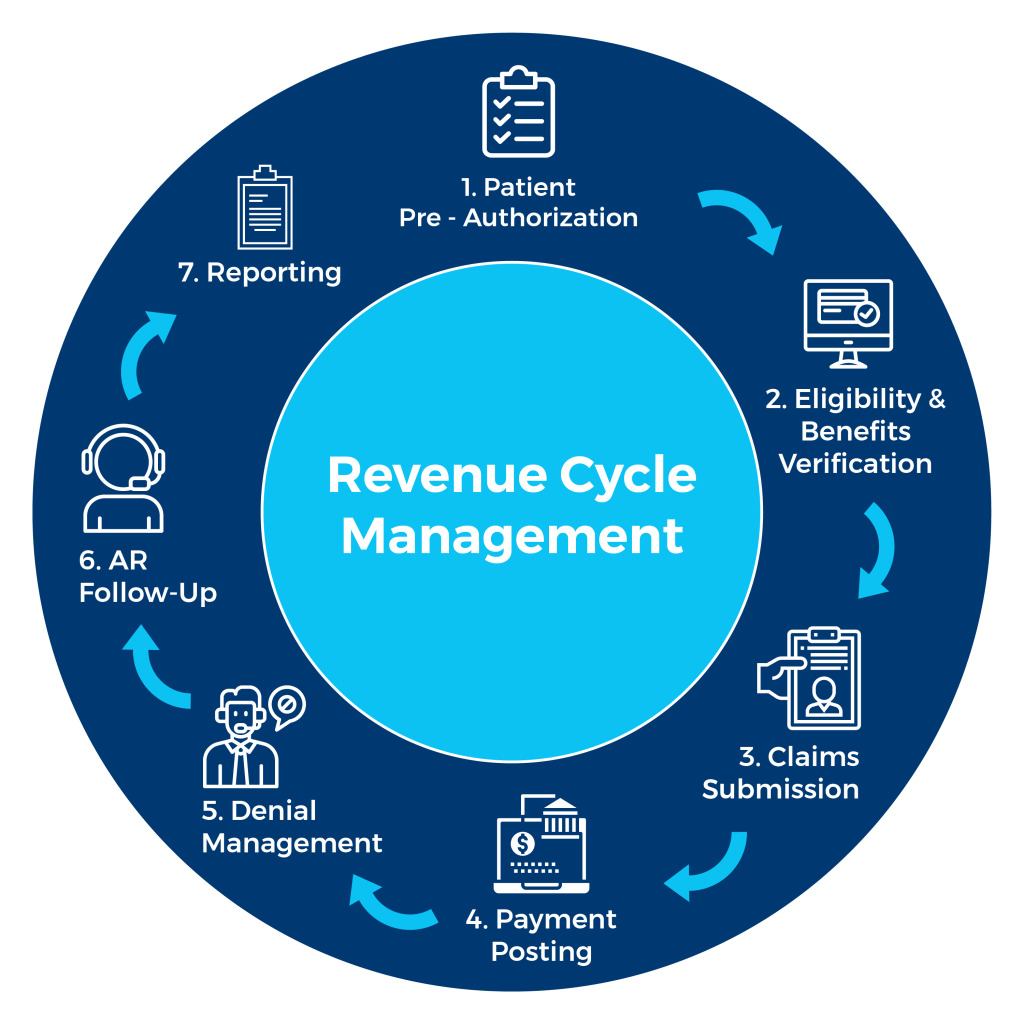
And so, since cash flow is the life blood of any healthcare revenue cycle management initiative, it is important for physician executives and healthcare administrators to appreciate the impact of modern health information technology systems on this vital function.
Functional Area Targets
Technology plays a key role across all health entity revenue cycle operations. By functional area, the following are key targets:
Patient Access
This is the front-end of a hospital’s revenue cycle. It is made up of all the pre-registration, registration, scheduling, pre-admitting, and admitting functions. Enhancing revenue cycles in this area requires the following:
-
a call center environment with auto dialing, faxing, and Internet connectivity to quickly ensure and verify all pertinent information that is key to correct and timely payment for services rendered;
-
Master Person Index software to eliminate duplicate medical record numbers and assist with achieving of a unique identifier for all patients;
-
registration and admission software that scripts the admission process to assist employees in obtaining required elements and check that insurer-required referrals are documented;
-
denial management definition, including focus on how to obtain all the correct patient information up front while the patient is in-house; and
-
imaging of data up front.
Health Information Management
This is the middle process of a hospital revenue cycle and is often still referred to as “Medical Records.” This area is made up of chart processing, coding, transcription, correspondence, and chart completion. Better control of revenue cycles requires the following recommended technology:
-
chart-tracking software to eliminate manual outguides and decrease the number of lost charts;
-
encoding and grouping software to improve coding accuracy and speed and improve reimbursement;
-
auto printing and faxing capabilities;
-
Internet connectivity for release of information and related document management tasks; and,
-
electronic management of documents.
Patient Financial Services
This is the back-end process of a hospital revenue cycle. The operations include all business office functions of billing, collecting, and follow-up post-patient care. Recommended technology to optimize these functions includes the following:
-
automated biller queues to improve and track the productivity of each biller;
-
claims scrubbing software to ensure that necessary data is included on the claim prior to submission; and
-
electronic claims and reimbursement processing to expedite the payment cycle.
Automation
Automation can lead to decreased paperwork, process standardization, increased productivity, and cleaner claims. In 2004, Hospital & Health Network’s “Most Wired Survey” found that the 100 most wired hospitals — including three out of the four AA+ hospitals in the country — had better control of expenses, higher productivity, and efficient utilization management. Today, these top hospitals tend to be larger and have better access to capital in these times of credit tightening.


Assessment
The positive return on investment in technology increases allocation of funding to technology. This correlation is important because it begins to link the investment in information technology with positive financial returns in all areas of a hospital’s business, including the revenue cycle.
MORE: Rev Cycle Mgmnt
Channel Surfing the ME-P
Have you visited our other topic channels? Established to facilitate idea exchange and link our community together, the value of these topics is dependent upon your input. Please take a minute to visit. And, to prevent that annoying spam, we ask that you register. It is fast, free and secure.
Conclusion
Your thoughts and comments on this ME-P are appreciated. Feel free to review our top-left column, and top-right sidebar materials, links, URLs and related websites, too. Then, subscribe to the ME-P. It is fast, free and secure.
Speaker: If you need a moderator or speaker for an upcoming event, Dr. David E. Marcinko; MBA – Publisher-in-Chief of the Medical Executive-Post – is available for seminar or speaking engagements. Contact: MarcinkoAdvisors@msn.com
OUR OTHER PRINT BOOKS AND RELATED INFORMATION SOURCES:



Filed under: Accounting, Healthcare Finance, iMBA, Inc., Information Technology, Managed Care | Tagged: cash flow, david marcinko, Healthcare Finance, hope hetico, Hospital Revenue Cycle Management, hospitals, karen white, profit augmentation, revenue cycle management | 3 Comments »