ACCOUNTABLE CARE ORGANIZATIONS
Realizing Equity, Access, and Community Health
By Staff Reporters
***
***
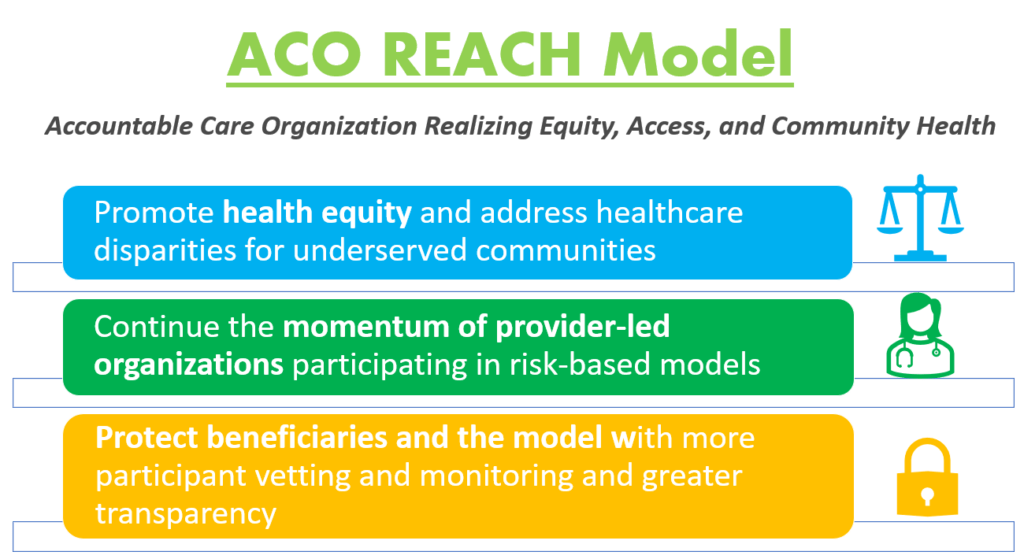
Model Overview
The ACO REACH Model provides novel tools and resources for health care providers to work together in an ACO to improve the quality of care for people with Traditional Medicare. REACH ACOs are comprised of different types of providers, including primary and specialty care physicians.
The ACO REACH Model makes important changes to the previous Global and Professional Direct Contracting (GPDC) Model which include:
***
***
- Promote Provider Leadership and Governance. The ACO REACH Model includes policies to ensure doctors and other health care providers continue to play a primary role in accountable care. At least 75% control of each ACO’s governing body generally must be held by participating providers or their designated representatives, compared to 25% during the first two Performance Years of the GPDC Model. In addition, the ACO REACH Model goes beyond prior ACO initiatives by requiring at least two beneficiary advocates on the governing board (at least one Medicare beneficiary and at least one consumer advocate), both of whom must hold voting rights.
- Protect Beneficiaries and the Model with More Participant Vetting, Monitoring and Greater Transparency. CMS will ask for additional information on applicants’ ownership, leadership, and governing board to gain better visibility into ownership interests and affiliations to ensure participants’ interests align with CMS’s vision. We will employ increased up-front screening of applicants, robust monitoring of participants, and greater transparency into the model’s progress during implementation, even before final evaluation results, and will share more information on the participants and their work to improve care. Last, CMS will also explore stronger protections against inappropriate coding and risk score growth.
MORE: https://www.cms.gov/priorities/innovation/innovation-models/aco-reach
COMMENTS APPRECIATED
Refer and Subscribe
***
***
Filed under: "Doctors Only", Accounting, Ethics, Health Economics, Health Insurance, Healthcare Finance, Practice Management, Quality Initiatives | Tagged: Access, Accountable Care Organization, ACO, ACO Reach, CDC, CMS, Community Health, DO, DPM, equity, GDPC, Global and Professional Direct Contracting, health equity, MD, Reach Model, Technology | Leave a comment »