By Dr. David Edward Marcinko MBA MEd
***
***
Shaping Well-being Beyond Medicine
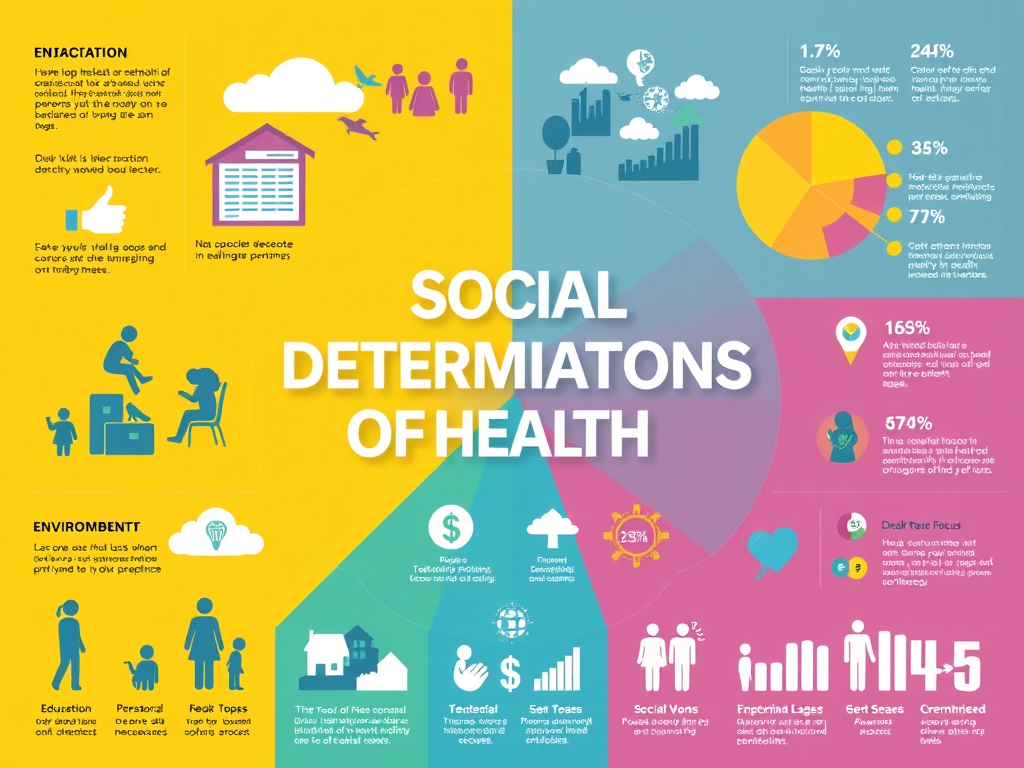
Health is often thought of as the result of medical care, but in reality, it is deeply influenced by the conditions in which people are born, grow, live, work, and age. These conditions, known as social determinants of health, include a wide range of social, economic, and environmental factors that shape health outcomes. They are responsible for many of the differences in health status between individuals and communities. Understanding these determinants is essential for promoting fairness in health and designing policies that reduce disparities.
Economic Stability
Economic stability is one of the most powerful determinants of health. Individuals with steady income can afford nutritious food, safe housing, and preventive healthcare. Conversely, poverty increases vulnerability to chronic diseases, mental health challenges, and limited access to medical services. Families with fewer financial resources may struggle to afford medications or healthy diets, leading to higher rates of obesity, diabetes, and cardiovascular disease. Unemployment or unstable work further exacerbates stress, which itself is linked to poor health outcomes. Economic inequality directly translates into health inequality.
Education
Education shapes health both directly and indirectly. Higher educational attainment is associated with better employment opportunities, higher income, and improved health literacy. People with more education are more likely to understand medical information, adopt healthy behaviors, and navigate healthcare systems effectively. Limited education can perpetuate cycles of poverty and poor health. For instance, children who grow up in underfunded schools may face restricted opportunities, leading to lower lifetime earnings and poorer health outcomes. Education is therefore a critical lever for breaking intergenerational cycles of disadvantage.
***
***
Neighborhood and Physical Environment
The environment in which individuals live plays a crucial role in determining health. Safe neighborhoods with clean air, accessible parks, and reliable transportation promote physical activity and reduce exposure to pollutants. In contrast, communities with high crime rates, poor housing, and environmental hazards contribute to stress, injury, and illness. Food deserts—areas with limited access to affordable, healthy food—are a striking example of how environment shapes health. Residents in these areas often rely on processed foods, increasing risks of obesity and related diseases. Housing quality also matters: overcrowding, mold, or lead exposure can lead to respiratory illnesses and developmental delays.
Healthcare Access and Quality
Access to healthcare is a fundamental determinant, but it is shaped by social and economic factors. Insurance coverage, affordability, and cultural competence of providers influence whether individuals receive timely and effective care. Marginalized groups often face barriers such as discrimination, language differences, or lack of nearby facilities. Even when healthcare is available, disparities in quality persist. For example, minority populations may receive less aggressive treatment for certain conditions compared to others. Addressing these inequities requires systemic reforms that prioritize inclusivity and affordability.
Social and Community Context
Social relationships and community support networks significantly affect health. Strong social ties provide emotional support, reduce stress, and encourage healthy behaviors. Communities with high levels of trust and civic engagement often experience better health outcomes. Conversely, discrimination, racism, and social exclusion undermine health by increasing stress and limiting opportunities. Social cohesion and equity are therefore vital for fostering healthier societies.
Conclusion
The social determinants of health highlight that medicine alone cannot ensure well-being. Economic stability, education, environment, healthcare access, and social context collectively shape health outcomes and drive disparities. Addressing these determinants requires a holistic approach that integrates public health, social policy, and community action. By investing in education, reducing poverty, improving neighborhoods, and ensuring equitable healthcare, societies can move closer to achieving health equity. Ultimately, health is not just about treating illness—it is about creating conditions in which everyone has the opportunity to thrive.
COMMENTS APPRECIATED
SPEAKING: Dr. Marcinko will be speaking and lecturing, signing and opining, teaching and preaching, storming and performing at many locations throughout the USA this year! His tour of witty and serious pontifications may be scheduled on a planned or ad-hoc basis; for public or private meetings and gatherings; formally, informally, or over lunch or dinner. All medical societies, financial advisory firms or Broker-Dealers are encouraged to submit an RFP for speaking engagements: CONTACT: Ann Miller RN MHA at MarcinkoAdvisors@outlook.com -OR- http://www.MarcinkoAssociates.com
Like, Refer and Subscribe
***
***
Filed under: "Doctors Only", Ask a Doctor, Glossary Terms, Health Economics, Health Insurance, Health Law & Policy, Healthcare Finance, Quality Initiatives, Touring with Marcinko | Tagged: david marcinko, Ethics, health, healthcare, mental health, Population Health, public health, SDH, social determinants health, wellness | Leave a comment »