Scrutiny Needed from the Patient Citizenry – Too?
As health care takes the center stage at the forefront of contemporary politics it is under scrutiny from several angles.
The Fraud Rate
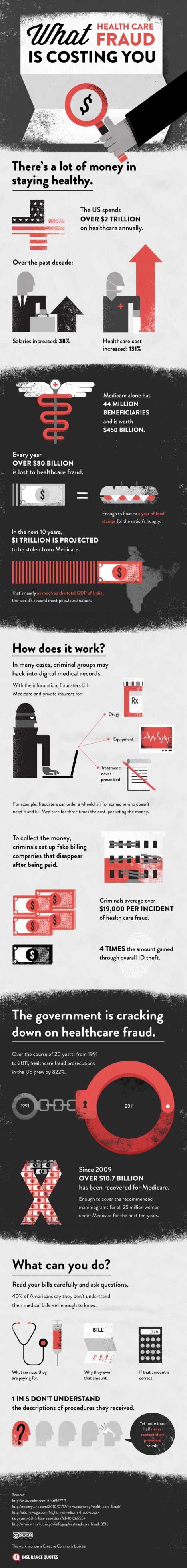
One aspect of the health care system that has been garnering growing levels of interest is the rate at which medical fraud occurs. As the developed world steeps itself further and further into the digital age, things like medical history and billing records become more easily susceptible to fraud since they’re accessible from virtually anywhere.
Expensive Care
And, the fact of the matter is that trying to stay healthy is an expensive business. Each year, 300 million Americans spend about $2 trillion on health care, but the amount of that money that is lost to fraud seems to have grown a great deal in recent years.
Types
The government continues to crack down and identify fraudsters in all their forms—and they do come in many forms. Perhaps the most common type of health care fraud concerns how medical care providers bill. This type of fraud relies heavily on the fact that many patients don’t take the proper amount of time to really scrutinize their medical bills and invoices.
Source: InsuranceQuotes.org
Assessment
Fraud can cost a huge amount of money for victim, insurance companies and society. The best defense against fraud remains understanding EOBs forms and what’s on your medical bills.
- Healthcare Fraud versus Healthcare Abuse
- New Pilot Program to Audit Hospital Bills
- Decoding Medical Bills [EOBs] for Laymen
Conclusion
Your thoughts and comments on this ME-P are appreciated. Feel free to review our top-left column, and top-right sidebar materials, links, URLs and related websites, too. Then, subscribe to the ME-P. It is fast, free and secure.
Speaker: If you need a moderator or speaker for an upcoming event, Dr. David E. Marcinko; MBA – Publisher-in-Chief of the Medical Executive-Post – is available for seminar or speaking engagements. Contact: MarcinkoAdvisors@msn.com
OUR OTHER PRINT BOOKS AND RELATED INFORMATION SOURCES:
- DICTIONARIES: http://www.springerpub.com/Search/marcinko
- PHYSICIANS: www.MedicalBusinessAdvisors.com
- PRACTICES: www.BusinessofMedicalPractice.com
- HOSPITALS: http://www.crcpress.com/product/isbn/9781466558731
- CLINICS: http://www.crcpress.com/product/isbn/9781439879900
- ADVISORS: www.CertifiedMedicalPlanner.org
- BLOG: www.MedicalExecutivePost.com
- FINANCE: Financial Planning for Physicians and Advisors
- INSURANCE: Risk Management and Insurance Strategies for Physicians and Advisors
Filed under: Ethics, Health Insurance, Health Law & Policy | Tagged: health abuse, health costs, health fraud |

















Affordable Care Act Will Crack Down on Medicare Fraud
The Obama administration has vowed to fight Medicare fraud and abuse. Included in the Affordable Care Act are provisions for more coordinated law enforcement actions; increased standards for medical providers, particularly in the medical equipment and supplies area; and the use of high-tech tools to better identify erroneous and fraudulent billing patterns.
The Centers for Medicare and Medicaid Services reported that $4.1 billion was recovered in 2011, a record amount for a single year. But despite the progress, Julie Schoen, Director of California’s Senior Medicare Patrol said, government and law enforcement agencies have a long way to go before they can catch up with the rampant abuse schemes.
Source: Walecia Konrad, New York Times [9/12/12]
LikeLike
Preventing Fraud in Your Practice
Fraud in the workplace costs U.S. employers approximately $600 billion a year, based on findings by the Association of Certified Fraud Examiners.
http://www.mdnews.com/news/2012_12/keep-your-practice-safe-from-fraud-and-embezzlement.aspx
While this malicious activity can happen in any workplace, your medical practice could be the site of such crimes, especially when it comes to elderly patients.
Ann Miller RN MHA
LikeLike
Dozens of patients of Oklahoma dentist test positive for hepatitis
The clinic of oral surgeon W. Scott Harrington was shut down in March after an investigation.
http://vitals.nbcnews.com/_news/2013/04/18/17813544-dozens-of-patients-of-oklahoma-dentist-test-positive-for-hepatitis?lite=
Why the cost may be more than just money.
Mary
LikeLike
Congressmen Question Reach of Fraud & Abuse Enforcement
During three recent hearings, various members of Congress openly questioned the scope and integrity of federal healthcare fraud and abuse enforcement, remarking that CMS and other federal agencies have created a “significant burden” on non-criminal providers through overreaching recovery audit programs that seek to reclaim improperly distributed funds from the Medicare program.
Click to access RAC.pdf
During recent hearings and discussions in the U.S. House of Representatives and U.S. Senate, legislators claimed that CMS recovery audit programs have created a 28-month backlog of over 450,000 appeals to CMS relating to coverage denials by Medicare auditors, which hinders the ability of providers to care for patients.
Robert James Cimasi MHA AVA CMP™
LikeLike
Health Care Fraud and Accrual Based Accounting
Let’s be truthful. “Sham Peer Review” is really ”Physician Peer Review Fraud”; according to Dr. Richard B Willner, the ED of the Center for Peer review Justice.
http://www.peerreviewsolutions.org/2011/09/07/health-care-fraud-and-accrual-based-accounting/
Health care fraud is a double entry system of accounting. We must discipline our thinking to reflect that of the accountant and lawyer so engaged in order to find the crooks and gather evidence of their misdeeds.
Hope R. Hetico RN MHA
LikeLike
Physicians Increasingly Targeted in Fraud & Abuse Lawsuits
In the midst of growing regulatory scrutiny regarding fraud and abuse, regulatory agencies are increasingly pursuing physicians, individually, under fraud and abuse laws.
In United States ex rel. Williams v. Banks-Jackson-Commerce Hosp. & Nursing Home Auth., a case stemming from the complaint of a relator (i.e., a private citizen) in the small community of Commerce, Georgia, a physician agreed to pay $200,000 to the U.S. to settle allegations regarding improper kickbacks in violation of the False Claims Act, Stark Law, and Anti-Kickback Statute.
While the settlement agreement, which was executed on September 22, 2014, led to the lawsuit’s dismissal, the announcement of the agreement is yet another sign of federal regulatory authorities utilizing a new tactic to boldly pursue fraud and abuse lawsuits, whereby individual physicians who receive improper payments may be liable under federal fraud and abuse laws.
Click to access PHYSICIANS.pdf
Robert James Cimasi MHA AVA CMP™
LikeLike