By Staff Reporters
Connection Makes the Difference – A Collaborative Shift in Bedside Manner?
Healthcare 2.0 is all about connecting. Take your pick: you can communicate via blogs, tweets, IMs, wikis, or social networks. And then, of course, you can opt for just plain old face-to-face dialogue.
The Communication Explosion
According to ME-P experts and Business of Medical Practice textbook contributors Mario Moussa PhD and Jennifer Tomasik MA, on the face of it, the explosion of communication options seems like a very good thing indeed.
www.BusinessofMedicalPractice.com
In the most basic ways, human beings need connection. Without the give and take of social interaction, our health suffers. In extreme situations—in solitary confinement or similar conditions—the brain almost completely shuts down.
What We Can Learn from Terry Anderson
The journalist Terry Anderson was held hostage in Lebanon from 1985 to 1992, enduring months at a time of almost complete isolation. In his memoir Den of Lions, Anderson described the catastrophic result: “The mind is a blank…. Where are all the things I learned, the books I read, the poems I memorized? There’s nothing there, just a formless, gray-black misery. My mind’s gone dead.”
The Link Between Social Connection and Good Health
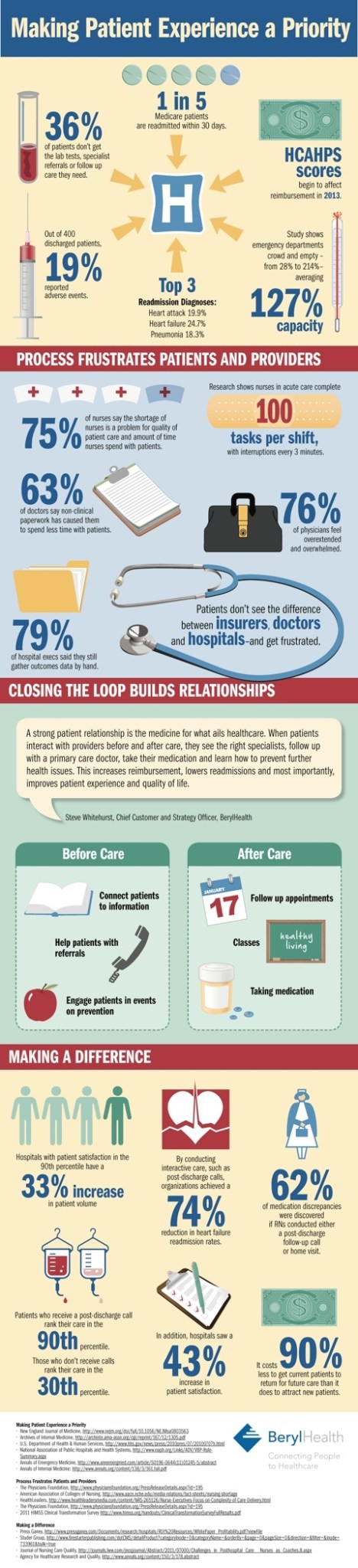
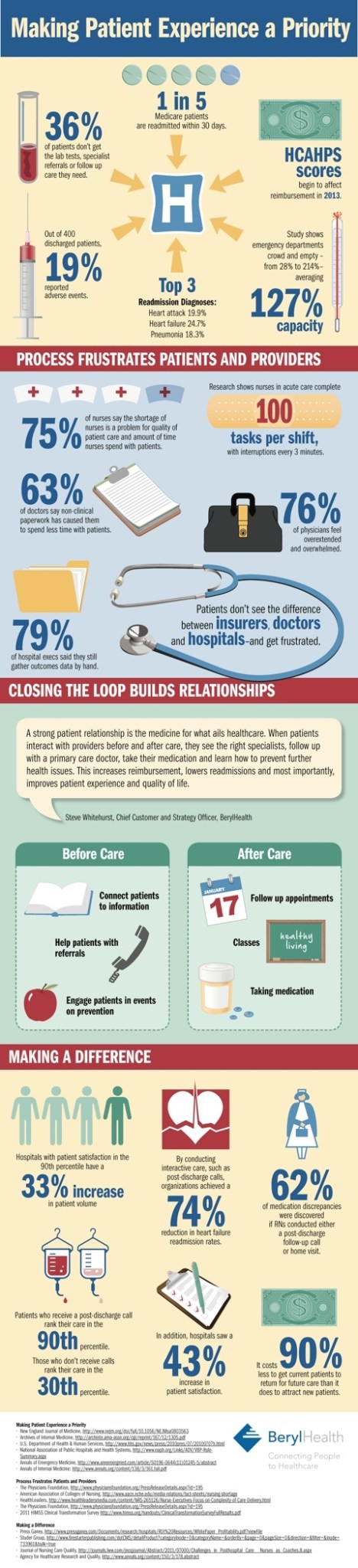
On the positive side, studies have established a link between social connection and good health. (Even contact with people you dislike is better than having no contact at all). The same goes for the relationship between doctor and patient: data show that when the relationship is satisfying, it has tangible health benefits.
For example, when patients have a positive emotional connection with their doctors, they remember a higher percentage of care-related information and even experience significantly better physiological outcomes.
The Conversation
And the way doctors converse with patients—apart from the actual content of the conversations—has an equally powerful effect:
Do you want your patient’s nagging headaches to go away?
Discuss their expectations and feelings, in addition to the neurological facts. This is much more effective than sticking to the facts alone, since a strong psychological bond is strong medicine.
Do you want your medical advice to be followed?
Draw your patient into conversations about treatment. The research shows that engagement makes a difference.
Assessment
Is there an analogy here for financial advisors and medical management consultants?
Conclusion
Your thoughts and comments on this ME-P are appreciated. Feel free to review our top-left column, and top-right sidebar materials, links, URLs and related websites, too. Then, subscribe to the ME-P. It is fast, free and secure.
Speaker: If you need a moderator or speaker for an upcoming event, Dr. David E. Marcinko; MBA – Publisher-in-Chief of the Medical Executive-Post – is available for seminar or speaking engagements. Contact: MarcinkoAdvisors@msn.com
OUR OTHER PRINT BOOKS AND RELATED INFORMATION SOURCES:



Filed under: Book Reviews, Information Technology, Practice Management, Quality Initiatives | Tagged: Business of Medical Practice, Jennifer Tomasik, Mario Moussa, Patient Experience, social media in medicine, www.BusinessofMedicalPractice.com | 5 Comments »