Pharmacy Benefits Management [PBM]
[By staff reporters]
DEFINITION:
In the United States, a pharmacy benefit manager (PBM) is a third-party administrator (TPA) of prescription drug programs for commercial health plans, self-insured employer plans, Medicare Part D plans, the Federal Employees Health Benefits Program (FEHBP), and state government employee plans. As of 2018 they have become industrial behemoths in the US health sector.
According to the American Pharmacists Association, “PBMs are primarily responsible for developing and maintaining the formulary, contracting with pharmacies, negotiating discounts and rebates with drug manufacturers, and processing and paying prescription drug claims.
For the most part, they work with self-insured companies and government programs striving to maintain or reduce the pharmacy expenditures of the plan while concurrently trying to improve health care outcomes”.
DICTIONARY
***
Now, read this: https://lnkd.in/eV2q2nB
Assessment
Your thoughts are appreciated.
***
***
HOSPITALS:
“Financial Management Strategies for Hospitals” https://tinyurl.com/yagu567d
“Operational Strategies for Clinics and Hospitals” https://tinyurl.com/y9avbrq5
***
Filed under: Drugs and Pharma | Tagged: PBMs |



















PBMs and Money
https://www.thecppc.com/single-post/2019/01/18/Boston-News-Channel-Digs-Into-PBMs-And-Where-the-Money-Is-Going
Inka
LikeLike
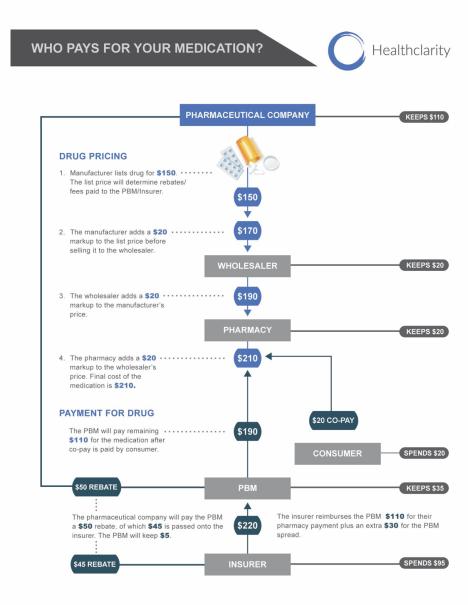
PBM’s Here’s how it works:
Makers of established brands give volume-based rebates to insurers or intermediaries called pharmacy benefit managers. In return, those middlemen often leave competing generics off the menu of drugs they cover, called a formulary, or they jack up the price for patients. The result is that many can’t get the cheaper drugs unless they shoulder a bigger copay or buy them with no help from insurance. Because rebate contracts are secret, nobody knows the full extent of the practice nor how much it costs the health system in unrealized savings.
“The deals between the drug companies and the PBM middle players are guarded as fiercely as Fort Knox,” said Robin Feldman, a law professor at the University of California, Hastings College of the Law, who studies pharma policy.”
https://khn.org/news/secretive-rebate-trap-keeps-generic-drugs-for-diabetes-and-other-ills-out-of-reach/
Cherry
LikeLike
PBMs
I wonder how many more states have to come forward telling how many hundreds of millions of dollars the PBM’s just TOOK, because they can! Before there are laws governing PBM’s !
https://www.statnews.com/pharmalot/2019/01/24/pharmacy-benefit-managers-spread-pricing-ny/
Jeff L.
LikeLike
On UHC
UnitedHealth expands program that requires drug discounts be passed on to consumer.
http://www.msn.com/en-us/money/insurance/unitedhealth-expands-program-that-requires-drug-discounts-be-passed-on-to-consumer/ar-BBUFm1f?li=BBnbfcN
Ginny
LikeLike
3 in 4 Health Systems Have an In-House Pharmacy
Aon recently released an analysis of their 2020 Benefits Survey of Hospitals. Here are some key findings on pharmacy plan requirements:
• 3 in 4 health systems have an in-house pharmacy.
• 11% of health systems require use of the in-house pharmacy for all medications.
• 12% require use of the in-house pharmacy for specialty medications only.
• 68% of health systems with an in-house pharmacy have no plan requirements.
Source: Aon, September 2020
LikeLike